কোষপতন: সংশোধিত সংস্করণের মধ্যে পার্থক্য
"Apoptosis" পাতাটি অনুবাদ করে তৈরি করা হয়েছে |
সম্পাদনা সারাংশ নেই |
||
| ১ নং লাইন: | ১ নং লাইন: | ||
{{short description|Programmed cell death in multicellular organisms}} |
|||
{{Infobox anatomy |
|||
| Name = Apoptosis |
|||
| Latin = |
|||
| Image = Apoptosis DU145 cells mosaic.jpg |
|||
| Caption = An [[etoposide]]-treated [[DU145|DU145 prostate cancer cell]] exploding into a cascade of apoptotic bodies. The sub images were extracted from a 61-hour [[time-lapse microscopy]] video, created using [[quantitative phase-contrast microscopy]]. The optical thickness is color-coded. With increasing thickness, color changes from gray to yellow, red, purple and finally black. [http://www.cellimagelibrary.org/images/43705<br />See the video at The Cell: An Image Library] |
|||
| Width = 306 |
|||
| Image2 = |
|||
| Caption2 = |
|||
| Precursor = |
|||
| System = |
|||
| Artery = |
|||
| Vein = |
|||
| Nerve = |
|||
| Lymph = |
|||
}} |
|||
[[File:Apoptosisgif.gif|thumb|Apoptosis begins when the nucleus of the cell begins to shrink. After the shrinking, the plasma membrane blebs and folds around different organelles. The blebs continue to form and the organelles fragment and move away from one another.]] |
|||
'''Apoptosis''' (from [[Ancient Greek]] [[wikt:ἀπόπτωσις|ἀπόπτωσις]], ''apóptōsis'', "falling off") is a form of [[programmed cell death]] that occurs in [[multicellular organism]]s.<ref>{{cite book |last=Green|first=Douglas | name-list-style = vanc |title=Means to an End: Apoptosis and other Cell Death Mechanisms|year=2011|publisher=Cold Spring Harbor Laboratory Press|location=Cold Spring Harbor, NY|isbn=978-0-87969-888-1|url=https://books.google.com/books?id=s8jBcQAACAAJ}}</ref> [[Biochemistry|Biochemical]] events lead to characteristic cell changes ([[Morphology (biology)|morphology]]) and death. These changes include [[Bleb (cell biology)|blebbing]], [[Plasmolysis|cell shrinkage]], [[Karyorrhexis|nuclear fragmentation]], [[Pyknosis|chromatin condensation]], [[Apoptotic DNA fragmentation|chromosomal DNA fragmentation]], and global{{vague|date = November 2017| reason= global in what sense: resulting from the intrinsic instability of all biology (anything whose stability is not dynamic is inert)? Or global to an idivdual in question, bcz their whole system is being challenged by their disease agent of the week? (hmm, am i overreaching, or is that an instance of Dylan's "He who is not busy living is busy dying?}} [[mRNA]] decay. The average adult human loses between 50 and 70 [[1,000,000,000|billion]] cells each day due to apoptosis.{{efn|Note that the average human adult has more than 13 trillion cells ({{val|1.3|e=13}}),{{sfn|Alberts|p=2}} of which at most only 70 billion ({{val|7.0|e=10}}) die per day. That is, about 5 out of every 1,000 cells (0.5%) die each day due to apoptosis.}} For an average human child between the ages of 8 and 14, approximately 20–30 billion cells die per day.<ref>{{cite book |last=Karam|first=Jose A. | name-list-style = vanc |title=Apoptosis in Carcinogenesis and Chemotherapy|year=2009|publisher=Springer|location=Netherlands|isbn=978-1-4020-9597-9}}</ref> |
|||
{{তথ্যছক শারীরস্থান|Name=Apoptosis|Latin=|Image=Apoptosis DU145 cells mosaic.jpg|Caption=An [[etoposide]]-treated [[DU145|DU145 prostate cancer cell]] exploding into a cascade of apoptotic bodies. The sub images were extracted from a 61-hour [[time-lapse microscopy]] video, created using [[quantitative phase-contrast microscopy]]. The optical thickness is color-coded. With increasing thickness, color changes from gray to yellow, red, purple and finally black. [http://www.cellimagelibrary.org/images/43705<br />See the video at The Cell: An Image Library]|Width=306|Image2=|Caption2=|precursor=|system=|Artery=|vein=|nerve=|lymph=}} |
|||
[[চিত্র:Apoptosisgif.gif|থাম্ব| কোষের নিউক্লিয়াস সঙ্কুচিত হতে শুরু করলে এপোপটোসিস শুরু হয়। সঙ্কুচিত হওয়ার পরে, প্লাজমা ঝিল্লিতে ছোটো ফোস্কা পড়ে আর বিভিন্ন অর্গানেলগুলির চারপাশে ভাঁজ হয়। ছোটো ফোস্কাগুলো অবিরত হতে থাকে এবং অর্গানেলস খণ্ড হয়ে ও একে অপরের থেকে দূরে সরে যায়।]] |
|||
In contrast to [[necrosis]], which is a form of traumatic cell death that results from acute cellular injury, apoptosis is a highly regulated and controlled process that confers advantages during an organism's life cycle. For example, the separation of fingers and toes in a developing human [[embryo]] occurs because cells between the digits undergo apoptosis. Unlike necrosis, apoptosis produces cell fragments called [[Extracellular vesicle#Apoptotic bodies|apoptotic bodies]] that [[phagocytic cells]] are able to engulf and remove before the contents of the cell can spill out onto surrounding cells and cause damage to them.<ref>{{cite book |last1=Alberts |first1=Bruce |last2=Johnson |first2=Alexander |last3=Lewis |first3=Julian |last4=Raff |first4=Martin |last5=Roberts |first5=Keith |last6=Walter |first6=Peter | name-list-style = vanc |title=Molecular Biology of the Cell (textbook) |edition=5th |publisher=[[Garland Science]] |page=1115 |chapter=Chapter 18 Apoptosis: Programmed Cell Death Eliminates Unwanted Cells |year=2008 |isbn=978-0-8153-4105-5|title-link=Molecular Biology of the Cell (textbook) }}</ref> |
|||
'''Apoptosis''' (থেকে [[প্রাচীন গ্রিক]] [[wiktionary:ἀπόπτωσις|ἀπόπτωσις]], ''apóptōsis,'' "খসে পড়া") [[বহুকোষী জীব|বহুকোষী প্রাণীদের]] ঘটা এক ধরনের প্রোগ্রাম কোষের মৃত্যু। <ref>{{বই উদ্ধৃতি|ইউআরএল=https://books.google.com/books?id=s8jBcQAACAAJ|শিরোনাম=Means to an End: Apoptosis and other Cell Death Mechanisms|শেষাংশ=Green|প্রথমাংশ=Douglas|বছর=2011|প্রকাশক=Cold Spring Harbor Laboratory Press|আইএসবিএন=978-0-87969-888-1}}</ref> [[প্রাণরসায়ন|বায়োকেমিক্যাল]] বিভিন্ন ঘটনা কোষের বৈশিষ্ট্যযুক্ত কিছু পরিবর্তন ( [[অঙ্গসংস্থান|রূপবিজ্ঞান]] ) করে এবং মৃত্যুর দিকে পরিচালিত করে। এই পরিবর্তনগুলির মধ্যে ব্লেব্বিং, সেল সংকোচন, পারমাণবিক খণ্ডন, ক্রোমাটিন ঘনীভবন, ক্রোমোজল ডিএনএ খণ্ডন এবং গ্লোবাল অন্তর্ভুক্ত রয়েছে [[বার্তাবাহী আরএনএ|এমআরএনএ]] ক্ষয় অ্যাপোপটোসিসের কারণে গড়ে প্রাপ্ত বয়স্ক মানুষ প্রতিদিন 50 থেকে 70 [[বিলিয়ন|বিলিয়ন কোষের মধ্যে হেরে যায়।]] {{Efn|Note that the average human adult has more than 13 trillion cells ({{val|1.3|e=13}}),{{sfn|Alberts|p=2}} of which at most only 70 billion ({{val|7.0|e=10}}) die per day. That is, about 5 out of every 1,000 cells (0.5%) die each day due to apoptosis.}} 8 থেকে 14 বছর বয়সের মধ্যে গড়ে গড়ে গড়ে আসা মানুষের শিশুদের জন্য প্রতিদিন প্রায় 20-30 কোটির কোষ মারা যায়। <ref>{{বই উদ্ধৃতি|শিরোনাম=Apoptosis in Carcinogenesis and Chemotherapy|শেষাংশ=Karam|প্রথমাংশ=Jose A.|বছর=2009|প্রকাশক=Springer|আইএসবিএন=978-1-4020-9597-9}}</ref>{{সূত্র তালিকা|35em}} |
|||
[[বিষয়শ্রেণী:চিকিৎসাবিজ্ঞানের প্রেক্ষাপটে মৃত্যু]] |
|||
Because apoptosis cannot stop once it has begun, it is a highly regulated process. Apoptosis can be initiated through one of two pathways. In the ''intrinsic pathway'' the cell kills itself because it senses [[Cellular stress response|cell stress]], while in the ''extrinsic pathway'' the cell kills itself because of signals from other cells. Weak external signals may also activate the intrinsic pathway of apoptosis.<ref>{{cite journal | vauthors = Raychaudhuri S | title = A minimal model of signaling network elucidates cell-to-cell stochastic variability in apoptosis | journal = PLOS ONE | volume = 5 | issue = 8 | pages = e11930 | date = August 2010 | pmid = 20711445 | pmc = 2920308 | doi = 10.1371/journal.pone.0011930 | bibcode = 2010PLoSO...511930R | arxiv = 1009.2294 }}</ref> Both pathways induce cell death by activating [[caspase]]s, which are [[protease]]s, or enzymes that degrade proteins. The two pathways both activate initiator caspases, which then activate executioner caspases, which then kill the cell by degrading proteins indiscriminately. |
|||
[[বিষয়শ্রেণী:অনাক্রম্যবিজ্ঞান]] |
|||
In addition to its importance as a biological phenomenon, defective apoptotic processes have been implicated in a wide variety of diseases. Excessive apoptosis causes [[atrophy]], whereas an insufficient amount results in uncontrolled cell proliferation, such as [[cancer]]. Some factors like [[Fas receptor]]s and caspases promote apoptosis, while some members of the [[Bcl-2 family]] of proteins inhibit apoptosis. |
|||
==Discovery and etymology== |
|||
{{Main|History of apoptosis research}} |
|||
German scientist [[Carl Vogt]] was first to describe the principle of apoptosis in 1842. In 1885, anatomist [[Walther Flemming]] delivered a more precise description of the process of programmed cell death. However, it was not until 1965 that the topic was resurrected. While studying tissues using electron microscopy, [[John Kerr (pathologist)|John Foxton Ross Kerr]] at the University of Queensland was able to distinguish apoptosis from traumatic cell death.<ref>{{cite journal | vauthors = Kerr JF | title = A histochemical study of hypertrophy and ischaemic injury of rat liver with special reference to changes in lysosomes | journal = The Journal of Pathology and Bacteriology | volume = 90 | issue = 2 | pages = 419–35 | date = October 1965 | pmid = 5849603 | doi = 10.1002/path.1700900210 }}</ref> Following the publication of a paper describing the phenomenon, Kerr was invited to join [[Alastair Currie|Alastair R. Currie]], as well as [[Andrew Wyllie]], who was Currie's graduate student,<ref name="AHW 1972">{{cite web|url=http://www.a-star.edu.sg/astar/biomed/action/biomed_dvp_abstract.do?id=2901ddeb02dH |title=Prof Andrew H. Wyllie – Lecture Abstract |access-date=2007-03-30 |authors=Agency for Science, Technology and Research |archive-url=https://web.archive.org/web/20071113101931/http://www.a-star.edu.sg/astar/biomed/action/biomed_dvp_abstract.do?id=2901ddeb02dH |archive-date=2007-11-13 |url-status=dead }}</ref> at University of Aberdeen. In 1972, the trio published a seminal article in the [[British Journal of Cancer]].<ref name="Kerr1972">{{cite journal | vauthors = Kerr JF, Wyllie AH, Currie AR | title = Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics | journal = British Journal of Cancer | volume = 26 | issue = 4 | pages = 239–57 | date = August 1972 | pmid = 4561027 | pmc = 2008650 | doi = 10.1038/bjc.1972.33 }}</ref> Kerr had initially used the term programmed cell necrosis, but in the article, the process of natural cell death was called ''apoptosis''. Kerr, Wyllie and Currie credited James Cormack, a professor of Greek language at [[University of Aberdeen]], with suggesting the term apoptosis. Kerr received the [[Paul Ehrlich and Ludwig Darmstaedter Prize]] on March 14, 2000, for his description of apoptosis. He shared the prize with Boston biologist [[H. Robert Horvitz]].<ref>{{cite journal | vauthors = O'Rourke MG, Ellem KA | title = John Kerr and apoptosis | journal = The Medical Journal of Australia | volume = 173 | issue = 11–12 | pages = 616–17 | year = 2000 | pmid = 11379508 | doi = 10.5694/j.1326-5377.2000.tb139362.x| s2cid = 38265127 | url = http://www.mja.com.au/public/issues/173_11_041200/orourke/orourke.html }}</ref> |
|||
For many years, neither "apoptosis" nor "programmed cell death" was a highly cited term. Two discoveries brought cell death from obscurity to a major field of research: identification of components of the cell death control and effector mechanisms, and linkage of abnormalities in cell death to human disease, in particular cancer. |
|||
The 2002 [[Nobel Prize in Physiology or Medicine|Nobel Prize in Medicine]] was awarded to [[Sydney Brenner]], Horvitz and [[John Sulston|John E. Sulston]] for their work identifying genes that control apoptosis. The genes were identified by studies in the nematode ''[[Caenorhabditis elegans|C. elegans]]'' and homologues of these genes function in humans to regulate apoptosis. |
|||
[[File:John Sulston.jpg|thumb|upright|[[John Sulston|John E. Sulston]] won the Nobel Prize in Medicine in 2002, for his pioneering research on apoptosis.]] |
|||
In Greek, apoptosis translates to the "falling off" of leaves from a tree.{{sfn|Alberts|p=1021}} Cormack, professor of Greek language, reintroduced the term for medical use as it had a medical meaning for the Greeks over two thousand years before. [[Hippocrates]] used the term to mean "the falling off of the bones". [[Galen]] extended its meaning to "the dropping of the scabs". Cormack was no doubt aware of this usage when he suggested the name. Debate continues over the correct pronunciation, with opinion divided between a pronunciation with the second ''p'' silent ({{IPAc-en|æ|p|ə|ˈ|t|oʊ|s|ᵻ|s}} {{respell|ap-ə|TOH|sis}}<ref name="bartleby.com">[http://www.bartleby.com/61/13/A0371350.html American Heritage Dictionary] {{webarchive |url=https://web.archive.org/web/20080630030923/http://www.bartleby.com/61/13/A0371350.html |date=June 30, 2008 }}</ref><ref name="aboutapop">{{cite web|url=http://www.nih.gov/sigs/aig/Aboutapo.html|title=About apoptosis|access-date=2006-12-15|year=1999|author=Apoptosis Interest Group|archive-url=https://web.archive.org/web/20061228100402/http://www.nih.gov/sigs/aig/Aboutapo.html|archive-date=28 December 2006|url-status=dead}}</ref>) and the second ''p'' pronounced ({{IPAc-en|ei|p|ə|p|ˈ|t|oʊ|s|ᵻ|s}}),<ref name="bartleby.com"/><ref name="webster.com">{{cite web|url=http://www.webster.com/dictionary/apoptosis|title=Definition of APOPTOSIS|website=www.webster.com|access-date=2007-08-11|archive-url=https://web.archive.org/web/20070703020311/http://webster.com/dictionary/apoptosis|archive-date=2007-07-03|url-status=dead}}</ref> as in the original Greek.{{Citation needed|date=May 2009}} In English, the ''p'' of the Greek ''-pt-'' [[consonant cluster]] is typically silent at the beginning of a word (e.g. [[Pterodactylus|pterodactyl]], [[Ptolemy]]), but articulated when used in combining forms preceded by a vowel, as in [[helicopter]] or the orders of insects: [[Fly|diptera]], [[lepidoptera]], etc. |
|||
In the original Kerr, Wyllie & Currie paper,<ref name=Kerr1972/> there is a footnote regarding the pronunciation: |
|||
<blockquote>We are most grateful to Professor James Cormack of the Department of Greek, University of Aberdeen, for suggesting this term. The word "apoptosis" ({{lang|grc|ἀπόπτωσις}}) is used in Greek to describe the "dropping off" or "falling off" of petals from flowers, or leaves from trees. To show the derivation clearly, we propose that the stress should be on the penultimate syllable, the second half of the word being pronounced like "ptosis" (with the "p" silent), which comes from the same root "to fall", and is already used to describe the drooping of the upper eyelid.</blockquote> |
|||
==Activation mechanisms== |
|||
[[File:Apoptosis.png|right]] |
|||
[[File:Control Of The Apoptosis Mecanisms.pdf|thumb|alt=Control Of The Apoptotic Mechanisms|Control Of The Apoptotic Mechanisms]] |
|||
The initiation of apoptosis is tightly regulated by activation mechanisms, because once apoptosis has begun, it inevitably leads to the death of the cell.{{sfn|Alberts|p=1029}}<ref name="pmid14499155">{{cite journal | vauthors = Böhm I, Schild H | title = Apoptosis: the complex scenario for a silent cell death | journal = Molecular Imaging and Biology | volume = 5 | issue = 1 | pages = 2–14 | year = 2003 | pmid = 14499155 | doi = 10.1016/S1536-1632(03)00024-6 }}</ref> The two best-understood activation mechanisms are the intrinsic pathway (also called the [[mitochondrial]] pathway) and the extrinsic pathway.{{sfn|Alberts|p=1023}} The ''intrinsic pathway'' is activated by intracellular signals generated when cells are stressed and depends on the release of proteins from the intermembrane space of mitochondria.{{sfn|Alberts|p=1032}} The ''extrinsic pathway'' is activated by extracellular ligands binding to cell-surface death receptors, which leads to the formation of the [[death-inducing signaling complex]] (DISC).{{sfn|Alberts|p=1024}} |
|||
A cell initiates intracellular apoptotic signaling in response to a stress,<ref>Nirmala GJ and Lopus M (2020) Cell death mechanisms in eukaryotes. Cell Biol Toxicol, 36, 145–164. doi: /10.1007/s10565-019-09496-2. {{PMID|31820165}}</ref> which may bring about cell suicide. The binding of nuclear receptors by [[glucocorticoid]]s,<ref name="robspath">{{cite book | title=Robbins Pathologic Basis of Disease| last1=Cotran | first1 = Ramzi S.| last2 = Kumar | first2 = Collins | name-list-style = vanc | publisher=W.B Saunders Company| location=Philadelphia| isbn=978-0-7216-7335-6 | year=1998 }}</ref> heat,<ref name="robspath"/> radiation,<ref name="robspath"/> nutrient deprivation,<ref name="robspath"/> viral infection,<ref name="robspath"/> [[Hypoxia (medical)|hypoxia]],<ref name="robspath"/> increased intracellular concentration of free fatty acids<ref>{{cite journal | vauthors = Hardy S, El-Assaad W, Przybytkowski E, Joly E, Prentki M, Langelier Y | title = Saturated fatty acid-induced apoptosis in MDA-MB-231 breast cancer cells. A role for cardiolipin | journal = The Journal of Biological Chemistry | volume = 278 | issue = 34 | pages = 31861–70 | date = August 2003 | pmid = 12805375 | doi = 10.1074/jbc.m300190200 | doi-access = free }}</ref> and increased intracellular [[calcium]] concentration,<ref name="pmid14647298">{{cite journal | vauthors = Mattson MP, Chan SL | title = Calcium orchestrates apoptosis | journal = Nature Cell Biology | volume = 5 | issue = 12 | pages = 1041–43 | date = December 2003 | pmid = 14647298 | doi = 10.1038/ncb1203-1041 | s2cid = 38427579 | url = https://zenodo.org/record/1233353 }}</ref><ref name="pmid19898892">{{cite journal | vauthors = Uğuz AC, Naziroğlu M, Espino J, Bejarano I, González D, Rodríguez AB, Pariente JA | title = Selenium modulates oxidative stress-induced cell apoptosis in human myeloid HL-60 cells through regulation of calcium release and caspase-3 and -9 activities | journal = The Journal of Membrane Biology | volume = 232 | issue = 1–3 | pages = 15–23 | date = December 2009 | pmid = 19898892 | doi = 10.1007/s00232-009-9212-2 | s2cid = 22215706 }}</ref> for example, by damage to the membrane, can all trigger the release of intracellular apoptotic signals by a damaged cell. A number of cellular components, such as [[poly ADP ribose polymerase]], may also help regulate apoptosis.<ref name="parp1">{{cite journal | vauthors = Chiarugi A, Moskowitz MA | title = Cell biology. PARP-1 – a perpetrator of apoptotic cell death? | journal = Science | volume = 297 | issue = 5579 | pages = 200–01 | date = July 2002 | pmid = 12114611 | doi = 10.1126/science.1074592 | s2cid = 82828773 }}</ref> Single cell fluctuations have been observed in experimental studies of stress induced apoptosis.<ref>{{cite journal | vauthors = Goldstein JC, Waterhouse NJ, Juin P, Evan GI, Green DR | title = The coordinate release of cytochrome c during apoptosis is rapid, complete and kinetically invariant | journal = Nature Cell Biology | volume = 2 | issue = 3 | pages = 156–62 | date = March 2000 | pmid = 10707086 | doi = 10.1038/35004029 | s2cid = 2283955 }}</ref><ref>{{cite journal | vauthors = Lee JK, Lu S, Madhukar A | title = Real-Time dynamics of Ca2+, caspase-3/7, and morphological changes in retinal ganglion cell apoptosis under elevated pressure | journal = PLOS ONE | volume = 5 | issue = 10 | pages = e13437 | date = October 2010 | pmid = 20976135 | pmc = 2956638 | doi = 10.1371/journal.pone.0013437 | bibcode = 2010PLoSO...513437L }}</ref> |
|||
Before the actual process of cell death is precipitated by enzymes, apoptotic signals must cause regulatory proteins to initiate the apoptosis pathway. This step allows those signals to cause cell death, or the process to be stopped, should the cell no longer need to die. Several proteins are involved, but two main methods of regulation have been identified: the targeting of [[Mitochondrion|mitochondria]] functionality,<ref>{{cite journal | vauthors = Bejarano I, Espino J, González-Flores D, Casado JG, Redondo PC, Rosado JA, Barriga C, Pariente JA, Rodríguez AB | title = Role of Calcium Signals on Hydrogen Peroxide-Induced Apoptosis in Human Myeloid HL-60 Cells | journal = International Journal of Biomedical Science | volume = 5 | issue = 3 | pages = 246–56 | date = September 2009 | pmid = 23675144 | pmc = 3614781 }}</ref> or directly transducing the signal via [[Signal transducing adaptor protein|adaptor proteins]] to the apoptotic mechanisms. An extrinsic pathway for initiation identified in several toxin studies is an increase in calcium concentration within a cell caused by drug activity, which also can cause apoptosis via a calcium binding protease [[calpain]]. |
|||
===Intrinsic pathway=== |
|||
The intrinsic pathway is also known as the mitochondrial pathway. [[Mitochondrion|Mitochondria]] are essential to multicellular life. Without them, a cell ceases to [[Cellular respiration#Aerobic respiration|respire aerobically]] and quickly dies. This fact forms the basis for some apoptotic pathways. Apoptotic proteins that target mitochondria affect them in different ways. They may cause mitochondrial swelling through the formation of membrane pores, or they may increase the permeability of the mitochondrial membrane and cause apoptotic effectors to leak out.<ref name="robspath"/><ref>{{cite journal|doi=10.2174/157436210791112172|title=Oxidative Stress-Induced Caspases are Regulated in Human Myeloid HL-60 Cells by Calcium Signal|journal=Current Signal Transduction Therapy|volume=5|issue=2|pages=181–186|year=2010|last1=Gonzalez|first1=D.|last2=Bejarano|first2=I.|last3=Barriga|first3=C.|last4=Rodriguez|first4=A.B.|last5=Pariente|first5=J.A.}}</ref> They are very closely related to intrinsic pathway, and [[tumors]] arise more frequently through intrinsic pathway than the extrinsic pathway because of sensitivity.<ref name="pmid20673794">{{cite journal | vauthors = Mohan S, Abdul AB, Abdelwahab SI, Al-Zubairi AS, Sukari MA, Abdullah R, Elhassan Taha MM, Ibrahim MY, Syam S | title = Typhonium flagelliforme induces apoptosis in CEMss cells via activation of caspase-9, PARP cleavage and cytochrome c release: its activation coupled with G0/G1 phase cell cycle arrest | journal = Journal of Ethnopharmacology | volume = 131 | issue = 3 | pages = 592–600 | date = October 2010 | pmid = 20673794 | doi = 10.1016/j.jep.2010.07.043 | url = http://psasir.upm.edu.my/id/eprint/9455/1/Typhonium%20flagelliforme%20induces%20apoptosis%20in%20CEMss%20cells%20via%20activation%20of%20caspase.pdf | access-date = 2019-07-05 | archive-url = https://web.archive.org/web/20190426134030/http://psasir.upm.edu.my/id/eprint/9455/1/Typhonium%20flagelliforme%20induces%20apoptosis%20in%20CEMss%20cells%20via%20activation%20of%20caspase.pdf | archive-date = 2019-04-26 | url-status = dead }}</ref> There is also a growing body of evidence indicating that [[nitric oxide]] is able to induce apoptosis by helping to dissipate the [[membrane potential]] of mitochondria and therefore make it more permeable.<ref name="NO">{{cite journal | vauthors = Brüne B | title = Nitric oxide: NO apoptosis or turning it ON? | journal = Cell Death and Differentiation | volume = 10 | issue = 8 | pages = 864–69 | date = August 2003 | pmid = 12867993 | doi = 10.1038/sj.cdd.4401261 | doi-access = free }}</ref> Nitric oxide has been implicated in initiating and inhibiting apoptosis through its possible action as a signal molecule of subsequent pathways that activate apoptosis.<ref>{{cite journal | vauthors = Brüne B, von Knethen A, Sandau KB | title = Nitric oxide (NO): an effector of apoptosis | journal = Cell Death and Differentiation | volume = 6 | issue = 10 | pages = 969–75 | date = October 1999 | pmid = 10556974 | doi = 10.1038/sj.cdd.4400582 | doi-access = free }}</ref> |
|||
During apoptosis, [[Cytochrome c|cytochrome ''c'']] is released from mitochondria through the actions of the proteins [[Bcl-2-associated X protein|Bax]] and [[Bcl-2 homologous antagonist killer|Bak]]. The mechanism of this release is enigmatic, but appears to stem from a multitude of Bax/Bak homo- and hetero-dimers of Bax/Bak inserted into the outer membrane.<ref>{{cite journal | vauthors = Uren RT, Iyer S, Kluck RM | title = Pore formation by dimeric Bak and Bax: an unusual pore? | journal = Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences | volume = 372 | issue = 1726 | pages = 20160218 | date = August 2017 | pmid = 28630157 | pmc = 5483520 | doi = 10.1098/rstb.2016.0218 }}</ref> Once cytochrome ''c'' is released it binds with Apoptotic protease activating factor – 1 (''[[Apaf-1]]'') and [[adenosine triphosphate|ATP]], which then bind to ''pro-caspase-9'' to create a protein complex known as an [[apoptosome]]. The apoptosome cleaves the pro-caspase to its active form of [[caspase-9]], which in turn cleaves and activates pro-caspase into the effector ''caspase-3''. |
|||
Mitochondria also release proteins known as SMACs (second mitochondria-derived activator of [[caspase]]s) into the cell's [[cytosol]] following the increase in permeability of the mitochondria membranes. SMAC binds to ''[[Inhibitor of apoptosis|proteins that inhibit apoptosis]]'' (IAPs) thereby deactivating them, and preventing the IAPs from arresting the process and therefore allowing apoptosis to proceed. IAP also normally suppresses the activity of a group of [[cysteine protease]]s called [[caspase]]s,<ref name="caspcontrol">{{cite journal | vauthors = Fesik SW, Shi Y | title = Structural biology. Controlling the caspases | journal = Science | volume = 294 | issue = 5546 | pages = 1477–78 | date = November 2001 | pmid = 11711663 | doi = 10.1126/science.1062236 | s2cid = 11392850 }}</ref> which carry out the degradation of the cell. Therefore, the actual degradation enzymes can be seen to be indirectly regulated by mitochondrial permeability. |
|||
===Extrinsic pathway=== |
|||
[[File:signal transduction pathways.png|thumb|500px|right|Overview of signal transduction pathways.]] |
|||
{{multiple image |
|||
| image1 = TFN-signalling.svg |
|||
| width1 = 250 |
|||
| image2 = Fas-signalling.svg |
|||
| width2 = 250 |
|||
| footer = Overview of TNF (left) and Fas (right) signalling in apoptosis, an example of direct signal transduction. |
|||
}} |
|||
Two theories of the direct initiation of apoptotic mechanisms in mammals have been suggested: the ''TNF-induced'' ([[tumor necrosis factor]]) model and the ''Fas-Fas [[ligand]]-mediated'' model, both involving receptors of the ''TNF receptor'' (TNFR) family<ref name="fas">{{cite journal | vauthors = Wajant H | title = The Fas signaling pathway: more than a paradigm | journal = Science | volume = 296 | issue = 5573 | pages = 1635–36 | date = May 2002 | pmid = 12040174 | doi = 10.1126/science.1071553 | bibcode = 2002Sci...296.1635W | s2cid = 29449108 }}</ref> coupled to extrinsic signals. |
|||
===TNF path=== |
|||
[[TNF-alpha]] is a [[cytokine]] produced mainly by activated [[macrophage]]s, and is the major extrinsic mediator of apoptosis. Most cells in the human body have two receptors for TNF-alpha: [[TNFR1]] and [[TNFR2]]. The binding of TNF-alpha to TNFR1 has been shown to initiate the pathway that leads to caspase activation via the intermediate membrane proteins TNF receptor-associated death domain ([[TRADD]]) and Fas-associated death domain protein ([[FADD]]). [[cIAP1]]/2 can inhibit TNF-α signaling by binding to [[TRAF2]]. [[CFLAR|FLIP]] inhibits the activation of caspase-8.<ref name="tnfr1">{{cite journal | vauthors = Chen G, Goeddel DV | s2cid = 25321662 | title = TNF-R1 signaling: a beautiful pathway | journal = Science | volume = 296 | issue = 5573 | pages = 1634–35 | date = May 2002 | pmid = 12040173 | doi = 10.1126/science.1071924 | bibcode = 2002Sci...296.1634C }}</ref> Binding of this receptor can also indirectly lead to the activation of [[transcription factor]]s involved in cell survival and inflammatory responses.<ref name="tfnpathway">{{cite journal | vauthors=Goeddel, DV| title=Connection Map for Tumor Necrosis Factor Pathway| journal=[[Science Signaling|Science's STKE]]| url=http://stke.sciencemag.org/cgi/cm/CMP_7107| doi = 10.1126/stke.3822007tw132| volume=2007| issue=382| pages=tw132| year=2007| s2cid=85404086}}</ref> However, signalling through TNFR1 might also induce apoptosis in a caspase-independent manner.<ref name="LAPFapoptosis">{{cite journal | vauthors = Chen W, Li N, Chen T, Han Y, Li C, Wang Y, He W, Zhang L, Wan T, Cao X | title = The lysosome-associated apoptosis-inducing protein containing the pleckstrin homology (PH) and FYVE domains (LAPF), representative of a novel family of PH and FYVE domain-containing proteins, induces caspase-independent apoptosis via the lysosomal-mitochondrial pathway | journal = The Journal of Biological Chemistry | volume = 280 | issue = 49 | pages = 40985–95 | date = December 2005 | pmid = 16188880 | doi = 10.1074/jbc.M502190200 | doi-access = free }}</ref> The link between TNF-alpha and apoptosis shows why an abnormal production of TNF-alpha plays a fundamental role in several human diseases, especially in [[autoimmune disease]]s. The [[TNF receptor superfamily|TNF-alpha receptor superfamily]] also includes death receptors (DRs), such as [[Death receptor 4|DR4]] and [[Death receptor 5|DR5]]. These receptors bind to the protein[[TRAIL]] and mediate apoptosis. Apoptosis is known to be one of the primary mechanisms of targeted cancer therapy.<ref>{{cite journal | vauthors = Gerl R, Vaux DL | title = Apoptosis in the development and treatment of cancer | journal = Carcinogenesis | volume = 26 | issue = 2 | pages = 263–70 | date = February 2005 | pmid = 15375012 | doi = 10.1093/carcin/bgh283 | doi-access = free }}</ref> Luminescent iridium complex-peptide hybrids (IPHs) have recently been designed, which mimic TRAIL and bind to death receptors on cancer cells, thereby inducing their apoptosis.<ref>{{cite journal | vauthors = Masum AA, Yokoi K, Hisamatsu Y, Naito K, Shashni B, Aoki S | title = Design and synthesis of a luminescent iridium complex-peptide hybrid (IPH) that detects cancer cells and induces their apoptosis | journal = Bioorganic & Medicinal Chemistry | volume = 26 | issue = 17 | pages = 4804–16 | date = September 2018 | pmid = 30177492 | doi = 10.1016/j.bmc.2018.08.016 }}</ref> |
|||
;Fas path |
|||
The [[fas receptor]] (First apoptosis signal) – (also known as ''Apo-1'' or ''CD95'') is a [[transmembrane protein]] of the TNF family which binds the [[FAS ligand|Fas ligand]] (FasL).<ref name="fas"/> The interaction between Fas and FasL results in the formation of the ''death-inducing signaling complex'' (DISC), which contains the FADD, caspase-8 and caspase-10. In some types of cells (type I), processed caspase-8 directly activates other members of the caspase family, and triggers the execution of apoptosis of the cell. In other types of cells (type II), the ''Fas''-DISC starts a feedback loop that spirals into increasing release of proapoptotic factors from mitochondria and the amplified activation of caspase-8.<ref name="fassignal">{{cite journal | vauthors = Wajant H | title=Connection Map for Fas Signaling Pathway| journal=[[Science Signaling|Science's STKE]]| url=http://stke.sciencemag.org/cgi/cm/CMP_7966 | doi = 10.1126/stke.3802007tr1 | volume=2007 | issue=380| pages=tr1| year=2007| s2cid=84909531}}</ref> |
|||
;Common components |
|||
Following ''TNF-R1'' and ''Fas'' activation in mammalian cells{{Citation needed|reason=This is only relevant Type II (pancreatic B-cells and hemaetapoetic stem cells), FAS depdnent apoptosis is indepdnent of MOMP|date=October 2020}} a balance between proapoptotic ([[Bcl-2-associated X protein|BAX]],<ref name="bax">{{cite journal | vauthors = Murphy KM, Ranganathan V, Farnsworth ML, Kavallaris M, Lock RB | title = Bcl-2 inhibits Bax translocation from cytosol to mitochondria during drug-induced apoptosis of human tumor cells | journal = Cell Death and Differentiation | volume = 7 | issue = 1 | pages = 102–11 | date = January 2000 | pmid = 10713725 | doi = 10.1038/sj.cdd.4400597 | author-link4 = Maria Kavallaris | doi-access = free }}</ref> [[BH3 interacting domain death agonist|BID]], [[Bcl-2 homologous antagonist killer|BAK]], or [[Bcl-2-associated death promoter|BAD]]) and anti-apoptotic (''[[Bcl-Xl]]'' and ''[[Bcl-2]]'') members of the ''Bcl-2'' family are established. This balance is the proportion of proapoptotic [[Protein dimer|homodimers]] that form in the outer-membrane of the mitochondrion. The proapoptotic homodimers are required to make the mitochondrial membrane permeable for the release of caspase activators such as cytochrome c and SMAC. Control of proapoptotic proteins under normal cell conditions of nonapoptotic cells is incompletely understood, but in general, Bax or Bak are activated by the activation of BH3-only proteins, part of the [[Bcl-2]] family{{Citation needed|reason=Not well agreed upon in recent reviews given BH3-only indepdnent Bax pore formation|date=October 2020}}. |
|||
;Caspases |
|||
[[Caspase]]s play the central role in the transduction of ER apoptotic signals. Caspases are proteins that are highly conserved, cysteine-dependent aspartate-specific proteases. There are two types of caspases: initiator caspases, caspase 2,8,9,10,11,12, and effector caspases, caspase 3,6,7. The activation of initiator caspases requires binding to specific oligomeric [[APAF1|activator protein]]. Effector caspases are then activated by these active initiator caspases through [[Proteolysis|proteolytic]] cleavage. The active effector caspases then proteolytically degrade a host of intracellular proteins to carry out the cell death program. |
|||
;Caspase-independent apoptotic pathway |
|||
There also exists a caspase-independent apoptotic pathway that is mediated by AIF ([[apoptosis-inducing factor]]).<ref name="pmid9989411">{{cite journal | vauthors = Susin SA, Lorenzo HK, Zamzami N, Marzo I, Snow BE, Brothers GM, Mangion J, Jacotot E, Costantini P, Loeffler M, Larochette N, Goodlett DR, Aebersold R, Siderovski DP, Penninger JM, Kroemer G | title = Molecular characterization of mitochondrial apoptosis-inducing factor | journal = Nature | volume = 397 | issue = 6718 | pages = 441–46 | date = February 1999 | pmid = 9989411 | doi = 10.1038/17135 | bibcode = 1999Natur.397..441S | s2cid = 204991081 }}</ref> |
|||
===Apoptosis model in amphibians=== |
|||
Amphibian frog ''[[Xenopus laevis]]'' serves as an ideal model system for the study of the mechanisms of apoptosis. In fact, iodine and thyroxine also stimulate the spectacular apoptosis of the cells of the larval gills, tail and fins in amphibians metamorphosis, and stimulate the evolution of their nervous system transforming the aquatic, vegetarian tadpole into the terrestrial, carnivorous [[frog]].<ref>{{cite journal | vauthors = Jewhurst K, Levin M, McLaughlin KA | title = Optogenetic Control of Apoptosis in Targeted Tissues of Xenopus laevis Embryos | journal = Journal of Cell Death | volume = 7 | pages = 25–31 | year = 2014 | pmid = 25374461 | pmc = 4213186 | doi = 10.4137/JCD.S18368 }}</ref><ref>{{Cite journal | last = Venturi | first = Sebastiano | name-list-style = vanc |title=Evolutionary Significance of Iodine |journal=Current Chemical Biology |volume=5 |pages=155–62 |year=2011 |doi=10.2174/187231311796765012 |issue=3}}</ref><ref>{{Cite journal |author=Venturi, Sebastiano |title=Iodine, PUFAs and Iodolipids in Health and Disease: An Evolutionary Perspective |journal=Human Evolution |volume= 29 |issue= 1–3 |pages=185–205 |year=2014 |issn=0393-9375}}</ref><ref>{{cite journal | vauthors = Tamura K, Takayama S, Ishii T, Mawaribuchi S, Takamatsu N, Ito M | title = Apoptosis and differentiation of Xenopus tail-derived myoblasts by thyroid hormone | journal = Journal of Molecular Endocrinology | volume = 54 | issue = 3 | pages = 185–92 | date = June 2015 | pmid = 25791374 | doi = 10.1530/JME-14-0327 | doi-access = free }}</ref> |
|||
== Negative regulators of apoptosis == |
|||
Negative regulation of apoptosis inhibits cell death signaling pathways, helping tumors to evade cell death and developing [[drug resistance]]. The ratio between anti-apoptotic (Bcl-2) and pro-apoptotic (Bax) proteins determines whether a cell lives or dies.<ref name="pmid31380246" /><ref name="pmid29149100">{{cite journal | vauthors = Kale J, Osterlund EJ, Andrews DW | title = BCL-2 family proteins: changing partners in the dance towards death | journal = [[Cell Death & Differentiation]] | volume = 25 | issue=1 | pages = 65–80 | date=2018 | doi = 10.1038/cdd.2017.186 | pmc=5729540 | pmid = 29149100}}</ref> Many families of proteins act as negative regulators categorized into either antiapoptotic factors, such as [[Inhibitor of apoptosis protein|IAPs]] and [[Bcl-2 family|Bcl-2]] proteins or prosurvival factors like [[CFLAR|cFLIP]], [[BNIP3]], [[FADD]], [[Protein kinase B|Akt]], and [[NF-κB]].<ref>{{cite journal | vauthors = Razaghi A, Heimann K, Schaeffer PM, Gibson SB | title = Negative regulators of cell death pathways in cancer: perspective on biomarkers and targeted therapies | journal = Apoptosis | volume = 23 | issue = 2 | pages = 93–112 | date = February 2018 | pmid = 29322476 | doi = 10.1007/s10495-018-1440-4 | s2cid = 3424489 }}</ref> |
|||
==Proteolytic caspase cascade: Killing the cell== |
|||
Many pathways and signals lead to apoptosis, but these converge on a single mechanism that actually causes the death of the cell. After a cell receives stimulus, it undergoes organized degradation of cellular organelles by activated proteolytic [[caspase]]s. In addition to the destruction of cellular organelles, [[mRNA]] is rapidly and globally degraded by a mechanism that is not yet fully characterized.<ref>{{cite journal | vauthors = Thomas MP, Liu X, Whangbo J, McCrossan G, Sanborn KB, Basar E, Walch M, Lieberman J | title = Apoptosis Triggers Specific, Rapid, and Global mRNA Decay with 3' Uridylated Intermediates Degraded by DIS3L2 | journal = Cell Reports | volume = 11 | issue = 7 | pages = 1079–89 | date = May 2015 | pmid = 25959823 | pmc = 4862650 | doi = 10.1016/j.celrep.2015.04.026 }}</ref> mRNA decay is triggered very early in apoptosis. |
|||
A cell undergoing apoptosis shows a series of characteristic morphological changes. Early alterations include: |
|||
# Cell shrinkage and rounding occur because of the retraction [[lamellipodia]] and the breakdown of the proteinaceous cytoskeleton by caspases.<ref>{{cite journal | vauthors = Böhm I | year = 2003 | title = Disruption of the cytoskeleton after apoptosis induction by autoantibodies | journal = Autoimmunity | volume = 36 | issue = 3| pages = 183–89 | doi=10.1080/0891693031000105617| pmid = 12911286 | s2cid = 37887253 }}</ref> |
|||
# The cytoplasm appears dense, and the organelles appear tightly packed. |
|||
# Chromatin undergoes condensation into compact patches against the [[Nuclear membrane|nuclear envelope]] (also known as the perinuclear envelope) in a process known as [[pyknosis]], a hallmark of apoptosis.<ref name="nuclearapopt">{{cite journal | vauthors = Susin SA, Daugas E, Ravagnan L, Samejima K, Zamzami N, Loeffler M, Costantini P, Ferri KF, Irinopoulou T, Prévost MC, Brothers G, Mak TW, Penninger J, Earnshaw WC, Kroemer G | title = Two distinct pathways leading to nuclear apoptosis | journal = The Journal of Experimental Medicine | volume = 192 | issue = 4 | pages = 571–80 | date = August 2000 | pmid = 10952727 | pmc = 2193229 | doi = 10.1084/jem.192.4.571 | display-authors = 6 }}</ref><ref name="chromatindegrad">{{cite journal | vauthors = Kihlmark M, Imreh G, Hallberg E | title = Sequential degradation of proteins from the nuclear envelope during apoptosis | journal = Journal of Cell Science | volume = 114 | issue = Pt 20 | pages = 3643–53 | date = October 2001 | pmid = 11707516 | url = http://jcs.biologists.org/cgi/content/full/114/20/3643 }}</ref> |
|||
# The nuclear envelope becomes discontinuous and the DNA inside it is fragmented in a process referred to as [[karyorrhexis]]. The nucleus breaks into several discrete ''chromatin bodies'' or ''nucleosomal units'' due to the degradation of DNA.<ref name="nuclearfrag">{{cite journal | vauthors = Nagata S | title = Apoptotic DNA fragmentation | journal = Experimental Cell Research | volume = 256 | issue = 1 | pages = 12–8 | date = April 2000 | pmid = 10739646 | doi = 10.1006/excr.2000.4834 }}</ref> |
|||
Apoptosis progresses quickly and its products are quickly removed, making it difficult to detect or visualize on classical histology sections. During karyorrhexis, [[endonuclease]] activation leaves short DNA fragments, regularly spaced in size. These give a characteristic "laddered" appearance on [[agar]] gel after [[electrophoresis]].<ref>{{cite journal | vauthors = Gong J, Traganos F, Darzynkiewicz Z | title = A selective procedure for DNA extraction from apoptotic cells applicable for gel electrophoresis and flow cytometry | journal = Analytical Biochemistry | volume = 218 | issue = 2 | pages = 314–19 | date = May 1994 | pmid = 8074286 | doi = 10.1006/abio.1994.1184 }}</ref> Tests for [[DNA laddering]] differentiate apoptosis from [[Ischemia|ischemic]] or toxic cell death.<ref name=Iwata>{{cite journal | vauthors = Iwata M, Myerson D, Torok-Storb B, Zager RA | title = An evaluation of renal tubular DNA laddering in response to oxygen deprivation and oxidant injury | journal = Journal of the American Society of Nephrology | volume = 5 | issue = 6 | pages = 1307–13 | date = December 1994 | pmid = 7893995 | url = http://jasn.asnjournals.org/cgi/content/abstract/5/6/1307 }}</ref> |
|||
===Apoptotic cell disassembly=== |
|||
[[File:Apoptotic cell disassembly.png|thumb|500px|Different steps in apoptotic cell disassembly.<ref>{{Cite journal|last1=Smith|first1=Aaron|last2=Parkes|first2=Michael AF|last3=Atkin-Smith|first3=Georgia K|last4=Tixeira|first4=Rochelle|last5=Poon|first5=Ivan KH | name-list-style = vanc |title=Cell disassembly during apoptosis|journal=WikiJournal of Medicine|language=en|volume=4|issue=1|doi=10.15347/wjm/2017.008|year=2017|doi-access=free}}</ref>]] |
|||
Before the apoptotic cell is disposed of, there is a process of disassembly. There are three recognized steps in apoptotic cell disassembly:<ref name="pmid28102458">{{cite journal | vauthors = Tixeira R, Caruso S, Paone S, Baxter AA, Atkin-Smith GK, Hulett MD, Poon IK | title = Defining the morphologic features and products of cell disassembly during apoptosis | journal = Apoptosis | volume = 22 | issue = 3 | pages = 475–77 | date = March 2017 | pmid = 28102458 | doi = 10.1007/s10495-017-1345-7 | s2cid = 34648758 }}</ref> |
|||
# Membrane blebbing: The cell membrane shows irregular buds known as [[bleb (cell biology)|blebs]]. Initially these are smaller surface blebs. Later these can grow into larger so-called dynamic membrane blebs.<ref name="pmid28102458"/> An important regulator of apoptotic cell membrane blebbing is [[ROCK1]] (rho associated coiled-coil-containing protein kinase 1).<ref name="pmid11283606">{{cite journal | vauthors = Coleman ML, Sahai EA, Yeo M, Bosch M, Dewar A, Olson MF | title = Membrane blebbing during apoptosis results from caspase-mediated activation of ROCK I | journal = Nature Cell Biology | volume = 3 | issue = 4 | pages = 339–45 | date = April 2001 | pmid = 11283606 | doi = 10.1038/35070009 | s2cid = 2537726 }}</ref><ref name="pmid11283607">{{cite journal | vauthors = Sebbagh M, Renvoizé C, Hamelin J, Riché N, Bertoglio J, Bréard J | title = Caspase-3-mediated cleavage of ROCK I induces MLC phosphorylation and apoptotic membrane blebbing | journal = Nature Cell Biology | volume = 3 | issue = 4 | pages = 346–52 | date = April 2001 | pmid = 11283607 | doi = 10.1038/35070019 | s2cid = 36187702 }}</ref> |
|||
# Formation of membrane protrusions: Some cell types, under specific conditions, may develop different types of long, thin extensions of the cell membrane called membrane protrusions. Three types have been described: [[microtubule]] spikes, '''apoptopodia''' (''feet of death''), and '''beaded apoptopodia''' (the latter having a beads-on-a-string appearance).<ref name="pmid16723742">{{cite journal | vauthors = Moss DK, Betin VM, Malesinski SD, Lane JD | title = A novel role for microtubules in apoptotic chromatin dynamics and cellular fragmentation | journal = Journal of Cell Science | volume = 119 | issue = Pt 11 | pages = 2362–74 | date = June 2006 | pmid = 16723742 | pmc = 1592606 | doi = 10.1242/jcs.02959 }}</ref><ref name="pmid24646995">{{cite journal | vauthors = Poon IK, Chiu YH, Armstrong AJ, Kinchen JM, Juncadella IJ, Bayliss DA, Ravichandran KS | title = Unexpected link between an antibiotic, pannexin channels and apoptosis | journal = Nature | volume = 507 | issue = 7492 | pages = 329–34 | date = March 2014 | pmid = 24646995 | pmc = 4078991 | doi = 10.1038/nature13147 | bibcode = 2014Natur.507..329P }}</ref><ref name="pmid26074490">{{cite journal | vauthors = Atkin-Smith GK, Tixeira R, Paone S, Mathivanan S, Collins C, Liem M, Goodall KJ, Ravichandran KS, Hulett MD, Poon IK | title = A novel mechanism of generating extracellular vesicles during apoptosis via a beads-on-a-string membrane structure | journal = Nature Communications | volume = 6 | pages = 7439 | date = June 2015 | pmid = 26074490 | pmc = 4490561 | doi = 10.1038/ncomms8439 | bibcode = 2015NatCo...6.7439A }}</ref> [[Pannexin 1]] is an important component of membrane channels involved in the formation of apoptopodia and beaded apoptopodia.<ref name="pmid24646995"/> |
|||
# [[Fragmentation (cell biology)|Fragmentation]]: The cell breaks apart into multiple [[Vesicle (biology and chemistry)|vesicles]] called ''apoptotic bodies'', which undergo [[phagocytosis]]. The plasma membrane protrusions may help bring apoptotic bodies closer to phagocytes. |
|||
===Removal of dead cells=== |
|||
The removal of dead cells by neighboring phagocytic cells has been termed [[efferocytosis]].<ref name="pmid16778289">{{cite journal | vauthors = Vandivier RW, Henson PM, Douglas IS | title = Burying the dead: the impact of failed apoptotic cell removal (efferocytosis) on chronic inflammatory lung disease | journal = Chest | volume = 129 | issue = 6 | pages = 1673–82 | date = June 2006 | pmid = 16778289 | doi = 10.1378/chest.129.6.1673 }}</ref> |
|||
Dying cells that undergo the final stages of apoptosis display phagocytotic molecules, such as [[phosphatidylserine]], on their cell surface.<ref name="Phosphatidylserine">{{cite journal | vauthors = Li MO, Sarkisian MR, Mehal WZ, Rakic P, Flavell RA | s2cid = 36252352 | title = Phosphatidylserine receptor is required for clearance of apoptotic cells | journal = Science | volume = 302 | issue = 5650 | pages = 1560–63 | date = November 2003 | pmid = 14645847 | doi = 10.1126/science.1087621 | bibcode = 2003Sci...302.1560O }}</ref> Phosphatidylserine is normally found on the inner leaflet surface of the plasma membrane, but is redistributed during apoptosis to the extracellular surface by a protein known as [[phospholipid scramblase|scramblase]].<ref name="phago2">{{cite journal | vauthors = Wang X, Wu YC, Fadok VA, Lee MC, Gengyo-Ando K, Cheng LC, Ledwich D, Hsu PK, Chen JY, Chou BK, Henson P, Mitani S, Xue D | title = Cell corpse engulfment mediated by C. elegans phosphatidylserine receptor through CED-5 and CED-12 | journal = Science | volume = 302 | issue = 5650 | pages = 1563–66 | date = November 2003 | pmid = 14645848 | doi = 10.1126/science.1087641 | url = http://ntur.lib.ntu.edu.tw/handle/246246/161415 | display-authors = 6 | bibcode = 2003Sci...302.1563W | s2cid = 25672278 }}</ref> These molecules mark the cell for [[phagocytosis]] by cells possessing the appropriate receptors, such as macrophages.<ref name="phago1">{{cite journal | vauthors = Savill J, Gregory C, Haslett C | s2cid = 13402617 | title = Cell biology. Eat me or die | journal = Science | volume = 302 | issue = 5650 | pages = 1516–17 | date = November 2003 | pmid = 14645835 | doi = 10.1126/science.1092533 | hdl = 1842/448 | hdl-access = free }}</ref> The removal of dying cells by phagocytes occurs in an orderly manner without eliciting an [[inflammatory response]].<ref name="phago1B">{{cite book | vauthors = Krysko DV, Vandenabeele P |title=Phagocytosis of dying cells: from molecular mechanisms to human diseases |url=https://www.springer.com/biomed/cancer/book/978-1-4020-9292-3 |isbn=978-1-4020-9292-3|date=2009-01-14 |publisher=Springer }}</ref> During apoptosis cellular RNA and DNA are separated from each other and sorted to different apoptotic bodies; separation of RNA is initiated as nucleolar segregation.<ref>{{cite journal | vauthors = Halicka HD, Bedner E, Darzynkiewicz Z | title = Segregation of RNA and separate packaging of DNA and RNA in apoptotic bodies during apoptosis | journal = Experimental Cell Research | volume = 260 | issue = 2 | pages = 248–56 | date = November 2000 | pmid = 11035919 | doi = 10.1006/excr.2000.5027 }}</ref> |
|||
==Pathway knock-outs== |
|||
Many [[gene knockout|knock-outs]] have been made in the apoptosis pathways to test the function of each of the proteins. Several caspases, in addition to [[APAF1]] and [[FADD]], have been mutated to determine the new phenotype. In order to create a tumor necrosis factor (TNF) knockout, an exon containing the nucleotides 3704–5364 was removed from the gene. This exon encodes a portion of the mature TNF domain, as well as the leader sequence, which is a highly conserved region necessary for proper intracellular processing. TNF-/- mice develop normally and have no gross structural or morphological abnormalities. However, upon immunization with SRBC (sheep red blood cells), these mice demonstrated a deficiency in the maturation of an antibody response; they were able to generate normal levels of IgM, but could not develop specific IgG levels. Apaf-1 is the protein that turns on caspase 9 by cleavage to begin the caspase cascade that leads to apoptosis. Since a -/- mutation in the APAF-1 gene is embryonic lethal, a gene trap strategy was used in order to generate an APAF-1 -/- mouse. This assay is used to disrupt gene function by creating an intragenic gene fusion. When an APAF-1 gene trap is introduced into cells, many morphological changes occur, such as spina bifida, the persistence of interdigital webs, and open brain. In addition, after embryonic day 12.5, the brain of the embryos showed several structural changes. APAF-1 cells are protected from apoptosis stimuli such as irradiation. A BAX-1 knock-out mouse exhibits normal forebrain formation and a decreased programmed cell death in some neuronal populations and in the spinal cord, leading to an increase in motor neurons. |
|||
The caspase proteins are integral parts of the apoptosis pathway, so it follows that knock-outs made have varying damaging results. A caspase 9 knock-out leads to a severe brain malformation. A caspase 8 knock-out leads to cardiac failure and thus embryonic lethality. However, with the use of cre-lox technology, a caspase 8 knock-out has been created that exhibits an increase in peripheral T cells, an impaired T cell response, and a defect in neural tube closure. These mice were found to be resistant to apoptosis mediated by CD95, TNFR, etc. but not resistant to apoptosis caused by UV irradiation, chemotherapeutic drugs, and other stimuli. Finally, a caspase 3 knock-out was characterized by ectopic cell masses in the brain and abnormal apoptotic features such as membrane blebbing or nuclear fragmentation. A remarkable feature of these KO mice is that they have a very restricted phenotype: Casp3, 9, APAF-1 KO mice have deformations of neural tissue and FADD and Casp 8 KO showed defective heart development, however, in both types of KO other organs developed normally and some cell types were still sensitive to apoptotic stimuli suggesting that unknown proapoptotic pathways exist. |
|||
==Methods for distinguishing apoptotic from necrotic (necroptotic) cells== |
|||
[[File:Apoptosis in mouse pre-adipocytes.gif|thumb|Long-term live cell imaging (12h) of multinucleated mouse pre-Adipocyte trying to undergo mitosis. Due to the excess of genetic material the cell fails to replicate and dies by apoptosis.]] |
|||
In order to perform analysis of apoptotic versus necrotic (necroptotic) cells, one can do analysis of morphology by label-free [[live cell imaging]], [[time-lapse microscopy]], [[flow cytometry|flow fluorocytometry]], and [[transmission electron microscopy]]. There are also various biochemical techniques for analysis of cell surface markers (phosphatidylserine exposure versus cell permeability by [[flow cytometry]]), cellular markers such as [[DNA fragmentation]]<ref>{{cite journal | vauthors = Lozano GM, Bejarano I, Espino J, González D, Ortiz A, García JF, Rodríguez AB, Pariente JA | year = 2009 | title = Density gradient capacitation is the most suitable method to improve fertilization and to reduce DNA fragmentation positive spermatozoa of infertile men | url = https://www.researchgate.net/publication/259983025 | journal = Anatolian Journal of Obstetrics & Gynecology | volume = 3 | issue = 1| pages = 1–7 }}</ref> (flow cytometry),<ref>{{cite journal | vauthors = Darzynkiewicz Z, Juan G, Li X, Gorczyca W, Murakami T, Traganos F | title = Cytometry in cell necrobiology: analysis of apoptosis and accidental cell death (necrosis) | journal = Cytometry | volume = 27 | issue = 1 | pages = 1–20 | date = January 1997 | pmid = 9000580 | doi = 10.1002/(sici)1097-0320(19970101)27:1<1::aid-cyto2>3.0.co;2-l | doi-access = free }}</ref> caspase activation, Bid cleavage, and cytochrome c release ([[Western blot]]ting). It is important to know how primary and secondary necrotic cells can be distinguished by analysis of [[supernatant]] for caspases, HMGB1, and release of cytokeratin 18. However, no distinct surface or biochemical markers of necrotic cell death have been identified yet, and only negative markers are available. These include absence of apoptotic markers (caspase activation, cytochrome c release, and oligonucleosomal DNA fragmentation) and differential kinetics of cell death markers (phosphatidylserine exposure and cell membrane permeabilization). A selection of techniques that can be used to distinguish apoptosis from necroptotic cells could be found in these references.<ref name="methods">{{cite book | vauthors = Krysko DV, Vanden Berghe T, Parthoens E, D'Herde K, Vandenabeele P | title = Methods for distinguishing apoptotic from necrotic cells and measuring their clearance | journal = Methods in Enzymology | volume = 442 | pages = 307–41 | year = 2008 | pmid = 18662577 | doi = 10.1016/S0076-6879(08)01416-X | isbn = 9780123743121 }}</ref><ref name="methods2">{{cite journal | vauthors = Krysko DV, Vanden Berghe T, D'Herde K, Vandenabeele P | title = Apoptosis and necrosis: detection, discrimination and phagocytosis | journal = Methods | volume = 44 | issue = 3 | pages = 205–21 | date = March 2008 | pmid = 18314051 | doi = 10.1016/j.ymeth.2007.12.001 }}</ref><ref name="methods3">{{cite journal | vauthors = Vanden Berghe T, Grootjans S, Goossens V, Dondelinger Y, Krysko DV, Takahashi N, Vandenabeele P | title = Determination of apoptotic and necrotic cell death in vitro and in vivo | journal = Methods | volume = 61 | issue = 2 | pages = 117–29 | date = June 2013 | pmid = 23473780 | doi = 10.1016/j.ymeth.2013.02.011 | url = https://zenodo.org/record/3423520 | access-date = 2019-11-05 | archive-url = https://web.archive.org/web/20191105075341/https://zenodo.org/record/3423520 | archive-date = 2019-11-05 | url-status = dead }}</ref><ref>{{cite book | vauthors = Wlodkowic D, Telford W, Skommer J, Darzynkiewicz Z | title = Recent Advances in Cytometry, Part B - Advances in Applications | chapter = Apoptosis and beyond: cytometry in studies of programmed cell death | journal = Methods in Cell Biology | volume = 103 | pages = 55–98 | year = 2011 | pmid = 21722800 | pmc = 3263828 | doi = 10.1016/B978-0-12-385493-3.00004-8 | isbn = 9780123854933 }}</ref> |
|||
==Implication in disease== |
|||
[[File:Apoptosis multi mouseliver.jpg|thumb|right|220px|A section of mouse liver showing several apoptotic cells, indicated by arrows]] |
|||
[[File:Apoptosis stained.jpg|thumb|right|220px|A section of mouse liver [[Staining (biology)|stained]] to show cells undergoing apoptosis (orange)]] |
|||
[[File:Apoptosis.jpg|thumb|right|220px|Neonatal cardiomyocytes ultrastructure after anoxia-reoxygenation.]] |
|||
===Defective pathways=== |
|||
The many different types of apoptotic pathways contain a multitude of different biochemical components, many of them not yet understood.<ref name="pathogenesis">{{cite journal | vauthors = Thompson CB | title = Apoptosis in the pathogenesis and treatment of disease | journal = Science | volume = 267 | issue = 5203 | pages = 1456–62 | date = March 1995 | pmid = 7878464 | doi = 10.1126/science.7878464 | bibcode = 1995Sci...267.1456T | s2cid = 12991980 }}</ref> As a pathway is more or less sequential in nature, removing or modifying one component leads to an effect in another. In a living organism, this can have disastrous effects, often in the form of disease or disorder. A discussion of every disease caused by modification of the various apoptotic pathways would be impractical, but the concept overlying each one is the same: The normal functioning of the pathway has been disrupted in such a way as to impair the ability of the cell to undergo normal apoptosis. This results in a cell that lives past its "use-by date" and is able to replicate and pass on any faulty machinery to its progeny, increasing the likelihood of the cell's becoming cancerous or diseased. |
|||
A recently described example of this concept in action can be seen in the development of a lung cancer called [[NCI-H460]].<ref name="h460">{{cite journal | vauthors = Yang L, Mashima T, Sato S, Mochizuki M, Sakamoto H, Yamori T, Oh-Hara T, Tsuruo T | title = Predominant suppression of apoptosome by inhibitor of apoptosis protein in non-small cell lung cancer H460 cells: therapeutic effect of a novel polyarginine-conjugated Smac peptide | journal = Cancer Research | volume = 63 | issue = 4 | pages = 831–37 | date = February 2003 | pmid = 12591734 | url = http://cancerres.aacrjournals.org/cgi/pmidlookup?view=long&pmid=12591734 }}</ref> The ''X-linked inhibitor of apoptosis protein'' ([[XIAP]]) is [[Gene expression|overexpressed]] in cells of the H460 [[cell line]]. XIAPs bind to the processed form of caspase-9, and suppress the activity of apoptotic activator [[cytochrome c]], therefore overexpression leads to a decrease in the amount of proapoptotic agonists. As a consequence, the balance of anti-apoptotic and proapoptotic effectors is upset in favour of the former, and the damaged cells continue to replicate despite being directed to die. Defects in regulation of apoptosis in cancer cells occur often at the level of control of transcription factors. As a particular example, defects in molecules that control transcription factor NF-κB in cancer change the mode of transcriptional regulation and the response to apoptotic signals, to curtail dependence on the tissue that the cell belongs. This degree of independence from external survival signals, can enable cancer metastasis.<ref>{{cite journal | vauthors = Vlahopoulos SA | title = Aberrant control of NF-κB in cancer permits transcriptional and phenotypic plasticity, to curtail dependence on host tissue: molecular mode | journal = Cancer Biology & Medicine | volume = 14 | issue = 3 | pages = 254–70 | date = August 2017 | pmid = 28884042 | pmc = 5570602 | doi = 10.20892/j.issn.2095-3941.2017.0029 }}</ref> |
|||
====Dysregulation of p53==== |
|||
The tumor-suppressor protein [[p53]] accumulates when DNA is damaged due to a chain of biochemical factors. Part of this pathway includes alpha-[[interferon]] and beta-interferon, which induce transcription of the ''p53'' gene, resulting in the increase of p53 protein level and enhancement of cancer cell-apoptosis.<ref name="takaoka">{{cite journal | vauthors = Takaoka A, Hayakawa S, Yanai H, Stoiber D, Negishi H, Kikuchi H, Sasaki S, Imai K, Shibue T, Honda K, Taniguchi T | display-authors = 6 | title = Integration of interferon-alpha/beta signalling to p53 responses in tumour suppression and antiviral defence | journal = Nature | volume = 424 | issue = 6948 | pages = 516–23 | date = July 2003 | pmid = 12872134 | doi = 10.1038/nature01850 | doi-access = free | bibcode = 2003Natur.424..516T }}</ref> p53 prevents the cell from replicating by stopping the [[cell cycle]] at G1, or interphase, to give the cell time to repair, however it will induce apoptosis if damage is extensive and repair efforts fail.<ref name="pmid12052432">{{cite journal | vauthors = Bernstein C, Bernstein H, Payne CM, Garewal H | title = DNA repair/pro-apoptotic dual-role proteins in five major DNA repair pathways: fail-safe protection against carcinogenesis | journal = Mutation Research | volume = 511 | issue = 2 | pages = 145–78 | date = June 2002 | pmid = 12052432 | doi = 10.1016/S1383-5742(02)00009-1 }}</ref> Any disruption to the regulation of the ''p53'' or interferon genes will result in impaired apoptosis and the possible formation of tumors. |
|||
===Inhibition=== |
|||
Inhibition of apoptosis can result in a number of cancers, inflammatory diseases, and viral infections. It was originally believed that the associated accumulation of cells was due to an increase in cellular proliferation, but it is now known that it is also due to a decrease in cell death. The most common of these diseases is cancer, the disease of excessive cellular proliferation, which is often characterized by an overexpression of [[inhibitor of apoptosis|IAP]] family members. As a result, the malignant cells experience an abnormal response to apoptosis induction: Cycle-regulating genes (such as p53, ras or c-myc) are mutated or inactivated in diseased cells, and further genes (such as bcl-2) also modify their expression in tumors. Some apoptotic factors are vital during mitochondrial respiration e.g. cytochrome C.<ref name="iopscience.iop.org">{{cite journal | vauthors = Kaczanowski S | year = 2016 | title = Apoptosis: its origin, history, maintenance and the medical implications for cancer and aging | url = http://eprints.ibb.waw.pl/1615/1/Apoptosis2016.pdf | journal = Phys Biol | volume = 13 | issue = 3 | page = 031001 | doi = 10.1088/1478-3975/13/3/031001 | pmid = 27172135 | bibcode = 2016PhBio..13c1001K | access-date = 2019-12-26 | archive-url = https://web.archive.org/web/20190428231913/http://eprints.ibb.waw.pl/1615/1/Apoptosis2016.pdf | archive-date = 2019-04-28 | url-status = dead }}</ref> Pathological inactivation of apoptosis in cancer cells is correlated with frequent respiratory metabolic shifts toward glycolysis (an observation known as the “Warburg hypothesis”.<ref name="Warburg_1956">{{cite journal | vauthors = Warburg O | title = On the origin of cancer cells | journal = Science | volume = 123 | issue = 3191 | pages = 309–14 | date = February 1956 | pmid = 13298683 | doi = 10.1126/science.123.3191.309 | bibcode = 1956Sci...123..309W }}</ref> |
|||
====HeLa cell==== |
|||
Apoptosis in [[HeLa]]{{efn|HeLa cells are an immortalized cancer cell line used frequently in research. The cell line was established by removing cells directly from [[Henrietta Lacks]], a cancer patient.}} cells is inhibited by proteins produced by the cell; these inhibitory proteins target retinoblastoma tumor-suppressing proteins.<ref name=DelPuerto/> These tumor-suppressing proteins regulate the cell cycle, but are rendered inactive when bound to an inhibitory protein.<ref name=DelPuerto/> HPV E6 and E7 are inhibitory proteins expressed by the human papillomavirus, HPV being responsible for the formation of the cervical tumor from which HeLa cells are derived.<ref name=Liu>{{cite journal | vauthors = Liu HC, Chen GG, Vlantis AC, Tse GM, Chan AT, van Hasselt CA | title = Inhibition of apoptosis in human laryngeal cancer cells by E6 and E7 oncoproteins of human papillomavirus 16 | journal = Journal of Cellular Biochemistry | volume = 103 | issue = 4 | pages = 1125–43 | date = March 2008 | pmid = 17668439 | doi = 10.1002/jcb.21490 | s2cid = 1651475 }}</ref> HPV E6 causes p53, which regulates the cell cycle, to become inactive.<ref name=Niu>{{cite journal | vauthors = Niu XY, Peng ZL, Duan WQ, Wang H, Wang P | title = Inhibition of HPV 16 E6 oncogene expression by RNA interference in vitro and in vivo | journal = International Journal of Gynecological Cancer | volume = 16 | issue = 2 | pages = 743–51 | year = 2006 | pmid = 16681755 | doi = 10.1111/j.1525-1438.2006.00384.x }}</ref> HPV E7 binds to retinoblastoma tumor suppressing proteins and limits its ability to control cell division.<ref name=Niu/> These two inhibitory proteins are partially responsible for HeLa cells' immortality by inhibiting apoptosis to occur.<ref name="Liu McKalip">{{cite journal | vauthors = Liu Y, McKalip A, Herman B | title = Human papillomavirus type 16 E6 and HPV-16 E6/E7 sensitize human keratinocytes to apoptosis induced by chemotherapeutic agents: roles of p53 and caspase activation | journal = Journal of Cellular Biochemistry | volume = 78 | issue = 2 | pages = 334–49 | date = May 2000 | pmid = 10842327 | doi = 10.1002/(sici)1097-4644(20000801)78:2<334::aid-jcb15>3.3.co;2-6 }}</ref> CDV (Canine Distemper Virus) is able to induce apoptosis despite the presence of these inhibitory proteins. This is an important [[Oncolytic virus|oncolytic]] property of CDV: this virus is capable of killing canine lymphoma cells. Oncoproteins E6 and E7 still leave p53 inactive, but they are not able to avoid the activation of caspases induced from the stress of viral infection. These oncolytic properties provided a promising link between CDV and lymphoma apoptosis, which can lead to development of alternative treatment methods for both canine [[lymphoma]] and human non-Hodgkin lymphoma. Defects in the cell cycle are thought to be responsible for the resistance to chemotherapy or radiation by certain tumor cells, so a virus that can induce apoptosis despite defects in the cell cycle is useful for cancer treatment.<ref name="Liu McKalip" /> |
|||
====Treatments==== |
|||
The main method of treatment for potential death from signaling-related diseases involves either increasing or decreasing the susceptibility of apoptosis in diseased cells, depending on whether the disease is caused by either the inhibition of or excess apoptosis. For instance, treatments aim to restore apoptosis to treat diseases with deficient cell death, and to increase the apoptotic threshold to treat diseases involved with excessive cell death. To stimulate apoptosis, one can increase the number of death receptor ligands (such as TNF or TRAIL), antagonize the anti-apoptotic Bcl-2 pathway, or introduce Smac mimetics to inhibit the inhibitor (IAPs).<ref name="pmid31380246">{{cite journal | vauthors = Jan R, Chaudhry G | title = Understanding Apoptosis and Apoptotic Pathways Targeted Cancer Therapeutics | journal = Advanced Pharmaceutical Bulletin | volume = 9 | issue=2 | pages = 205–218 | date=2019 | doi = 10.15171/apb.2019.024 | pmc=6664112 | pmid = 31380246}}</ref> The addition of agents such as Herceptin, Iressa, or Gleevec works to stop cells from cycling and causes apoptosis activation by blocking growth and survival signaling further upstream. Finally, adding p53-[[MDM2]] complexes displaces p53 and activates the p53 pathway, leading to cell cycle arrest and apoptosis. Many different methods can be used either to stimulate or to inhibit apoptosis in various places along the death signaling pathway.<ref>{{cite journal | vauthors = Boehm I | title = Apoptosis in physiological and pathological skin: implications for therapy | journal = Current Molecular Medicine | volume = 6 | issue = 4 | pages = 375–94 | date = June 2006 | pmid = 16900661 | doi = 10.2174/156652406777435390 }}</ref> |
|||
Apoptosis is a multi-step, multi-pathway cell-death programme that is inherent in every cell of the body. In cancer, the apoptosis cell-division ratio is altered. Cancer treatment by chemotherapy and irradiation kills target cells primarily by inducing apoptosis. |
|||
===Hyperactive apoptosis=== |
|||
On the other hand, loss of control of cell death (resulting in excess apoptosis) can lead to neurodegenerative diseases, hematologic diseases, and tissue damage. It is of interest to note that neurons that rely on mitochondrial respiration undergo apoptosis in neurodegenerative diseases such as Alzheimer's<ref name="pmid7704018">{{cite journal | vauthors = LaFerla FM, Tinkle BT, Bieberich CJ, Haudenschild CC, Jay G | title = The Alzheimer's A beta peptide induces neurodegeneration and apoptotic cell death in transgenic mice | journal = Nature Genetics | volume = 9 | issue = 1 | pages = 21–30 | date = January 1995 | pmid = 7704018 | doi = 10.1038/ng0195-21 | s2cid = 20016461 }}</ref> and Parkinson's.<ref name="pmid8782165">{{cite journal | vauthors = Mochizuki H, Goto K, Mori H, Mizuno Y | title = Histochemical detection of apoptosis in Parkinson's disease | journal = Journal of the Neurological Sciences | volume = 137 | issue = 2 | pages = 120–3 | date = May 1996 | pmid = 8782165 | doi = 10.1016/0022-510X(95)00336-Z| s2cid = 44329454 }}</ref> (an observation known as the “Inverse Warburg hypothesis” <ref name="pmid25642192">{{cite journal | vauthors = Demetrius LA, Magistretti PJ, Pellerin L | title = Alzheimer's disease: the amyloid hypothesis and the Inverse Warburg effect | journal = Frontiers in Physiology | volume = 5 | pages = 522 | date = 2014 | pmid = 25642192 | pmc = 4294122 | doi = 10.3389/fphys.2014.00522 }}</ref><ref name="iopscience.iop.org"/> ). Moreover, there is an inverse epidemiological comorbidity between neurodegenerative diseases and cancer.<ref name="pmid23843468">{{cite journal | vauthors = Musicco M, Adorni F, Di Santo S, Prinelli F, Pettenati C, Caltagirone C, Palmer K, Russo A | title = Inverse occurrence of cancer and Alzheimer disease: a population-based incidence study | journal = Neurology | volume = 81 | issue = 4 | pages = 322–8 | date = July 2013 | pmid = 23843468 | doi = 10.1212/WNL.0b013e31829c5ec1 | s2cid = 22792702 }}</ref> The progression of HIV is directly linked to excess, unregulated apoptosis. In a healthy individual, the number of CD4+ lymphocytes is in balance with the cells generated by the bone marrow; however, in HIV-positive patients, this balance is lost due to an inability of the bone marrow to regenerate CD4+ cells. In the case of HIV, CD4+ lymphocytes die at an accelerated rate through uncontrolled apoptosis, when stimulated. |
|||
At the molecular level, hyperactive apoptosis can be caused by defects in signaling pathways that regulate the Bcl-2 family proteins. Increased expression of apoptotic proteins such as BIM, or their decreased proteolysis, leads to cell death, and can cause a number of pathologies, depending on the cells where excessive activity of BIM occurs. Cancer cells can escape apoptosis through mechanisms that suppress BIM expression or by increased proteolysis of BIM.{{Citation needed|date=December 2019|reason=removed citation to predatory publisher content}} |
|||
====Treatments==== |
|||
Treatments aiming to inhibit works to block specific caspases. Finally, the Akt protein kinase promotes cell survival through two pathways. Akt phosphorylates and inhibits Bad (a Bcl-2 family member), causing Bad to interact with the [[14-3-3]] scaffold, resulting in Bcl dissociation and thus cell survival. Akt also activates IKKα, which leads to NF-κB activation and cell survival. Active NF-κB induces the expression of anti-apoptotic genes such as Bcl-2, resulting in inhibition of apoptosis. NF-κB has been found to play both an antiapoptotic role and a proapoptotic role depending on the stimuli utilized and the cell type.<ref name="Farhana_2005">{{cite journal | vauthors = Farhana L, Dawson MI, Fontana JA | title = Apoptosis induction by a novel retinoid-related molecule requires nuclear factor-kappaB activation | journal = Cancer Research | volume = 65 | issue = 11 | pages = 4909–17 | date = June 2005 | pmid = 15930313 | doi = 10.1158/0008-5472.CAN-04-4124 | doi-access = free }}</ref> |
|||
===HIV progression=== |
|||
The progression of the [[human immunodeficiency virus]] infection into [[AIDS]] is due primarily to the depletion of [[T helper cell|CD4+ T-helper lymphocytes]] in a manner that is too rapid for the body's bone marrow to replenish the cells, leading to a compromised immune system. One of the mechanisms by which T-helper cells are depleted is apoptosis, which results from a series of biochemical pathways:<ref name="Judie">{{cite journal | vauthors = Alimonti JB, Ball TB, Fowke KR | title = Mechanisms of CD4+ T lymphocyte cell death in human immunodeficiency virus infection and AIDS | journal = The Journal of General Virology | volume = 84 | issue = Pt 7 | pages = 1649–61 | date = July 2003 | pmid = 12810858 | doi = 10.1099/vir.0.19110-0 | doi-access = free }}</ref> |
|||
# HIV enzymes deactivate anti-apoptotic ''Bcl-2''. This does not directly cause cell death but primes the cell for apoptosis should the appropriate signal be received. In parallel, these enzymes activate proapoptotic ''procaspase-8'', which does directly activate the mitochondrial events of apoptosis. |
|||
# HIV may increase the level of cellular proteins that prompt Fas-mediated apoptosis. |
|||
# HIV proteins decrease the amount of [[CD4]] glycoprotein marker present on the cell membrane. |
|||
# Released viral particles and proteins present in extracellular fluid are able to induce apoptosis in nearby "bystander" T helper cells. |
|||
# HIV decreases the production of molecules involved in marking the cell for apoptosis, giving the virus time to replicate and continue releasing apoptotic agents and virions into the surrounding tissue. |
|||
# The infected CD4+ cell may also receive the death signal from a cytotoxic T cell. |
|||
Cells may also die as direct consequences of viral infections. HIV-1 expression induces tubular cell G2/M arrest and apoptosis.<ref>{{cite journal|doi=10.1080/08860220802134672|pmid=18661417|title=HIV-1 Expression Induces Tubular Cell G2/M Arrest and Apoptosis|journal=Renal Failure|volume=30|issue=6|pages=655–664|year=2008|last1=Vashistha|first1=Himanshu|last2=Husain|first2=Mohammad|last3=Kumar|first3=Dileep|last4=Yadav|first4=Anju|last5=Arora|first5=Shitij|last6=Singhal|first6=Pravin C.|doi-access=free}}</ref> The progression from HIV to AIDS is not immediate or even necessarily rapid; HIV's cytotoxic activity toward CD4+ lymphocytes is classified as AIDS once a given patient's CD4+ cell count falls below 200.<ref>{{cite web |author=Indiana University Health |url=http://iuhealth.org/riley/infectious-diseases/hiv/aids-defining-criteria/ |title=AIDS Defining Criteria | Riley |publisher=IU Health |access-date=2013-01-20 |archive-url=https://web.archive.org/web/20130526052627/http://iuhealth.org/riley/infectious-diseases/hiv/aids-defining-criteria/# |archive-date=2013-05-26 |url-status=dead }}</ref> |
|||
Researchers from Kumamoto University in Japan have developed a new method to eradicate HIV in viral reservoir cells, named "Lock-in and apoptosis." Using the synthesized compound Heptanoylphosphatidyl L-Inositol Pentakisphophate (or L-Hippo) to bind strongly to the HIV protein PR55Gag, they were able to suppress viral budding. By suppressing viral budding, the researchers were able to trap the HIV virus in the cell and allow for the cell to undergo apoptosis (natural cell death). Associate Professor Mikako Fujita has stated that the approach is not yet available to HIV patients because the research team has to conduct further research on combining the drug therapy that currently exists with this "Lock-in and apoptosis" approach to lead to complete recovery from HIV.<ref>{{cite journal | vauthors = Tateishi H, Monde K, Anraku K, Koga R, Hayashi Y, Ciftci HI, DeMirci H, Higashi T, Motoyama K, Arima H, Otsuka M, Fujita M | title = A clue to unprecedented strategy to HIV eradication: "Lock-in and apoptosis" | journal = Scientific Reports | volume = 7 | issue = 1 | pages = 8957 | date = August 2017 | pmid = 28827668 | pmc = 5567282 | doi = 10.1038/s41598-017-09129-w | bibcode = 2017NatSR...7.8957T }}</ref> |
|||
===Viral infection=== |
|||
Viral induction of apoptosis occurs when one or several cells of a living organism are<!--plural predicate to agree with "cells"--> infected with a [[virus]], leading to cell death. Cell death in organisms is necessary for the normal development of cells and the cell cycle maturation.<ref name=Indran>{{cite journal | vauthors = Indran IR, Tufo G, Pervaiz S, Brenner C | title = Recent advances in apoptosis, mitochondria and drug resistance in cancer cells | journal = Biochimica et Biophysica Acta (BBA) - Bioenergetics | volume = 1807 | issue = 6 | pages = 735–45 | date = June 2011 | pmid = 21453675 | doi = 10.1016/j.bbabio.2011.03.010 }}</ref> It is also important in maintaining the regular functions and activities of cells. |
|||
Viruses can trigger apoptosis of infected cells via a range of mechanisms including: |
|||
* Receptor binding |
|||
* Activation of [[protein kinase R]] (PKR) |
|||
* Interaction with p53 |
|||
* Expression of viral proteins coupled to MHC proteins on the surface of the infected cell, allowing recognition by cells of the immune system (such as [[Natural killer cell|Natural Killer]] and [[cytotoxic T cell]]s) that then induce the infected cell to undergo apoptosis.<ref name=Everett>{{cite journal | vauthors = Everett H, McFadden G | title = Apoptosis: an innate immune response to virus infection | journal = Trends in Microbiology | volume = 7 | issue = 4 | pages = 160–65 | date = April 1999 | pmid = 10217831 | doi = 10.1016/S0966-842X(99)01487-0 }}</ref> |
|||
[[Canine distemper virus]] (CDV) is known to cause apoptosis in central nervous system and lymphoid tissue of infected dogs in vivo and in vitro.<ref name=Nishi>{{cite journal | vauthors = Nishi T, Tsukiyama-Kohara K, Togashi K, Kohriyama N, Kai C | title = Involvement of apoptosis in syncytial cell death induced by canine distemper virus | journal = Comparative Immunology, Microbiology and Infectious Diseases | volume = 27 | issue = 6 | pages = 445–55 | date = November 2004 | pmid = 15325517 | doi = 10.1016/j.cimid.2004.01.007 }}</ref> |
|||
Apoptosis caused by CDV is typically induced via the [[death-inducing signaling complex|extrinsic pathway]], which activates [[caspases]] that disrupt cellular function and eventually leads to the cells death.<ref name=DelPuerto>{{cite journal | vauthors = Del Puerto HL, Martins AS, Milsted A, Souza-Fagundes EM, Braz GF, Hissa B, Andrade LO, Alves F, Rajão DS, Leite RC, Vasconcelos AC | title = Canine distemper virus induces apoptosis in cervical tumor derived cell lines | journal = Virology Journal | volume = 8 | issue = 1 | pages = 334 | date = June 2011 | pmid = 21718481 | pmc = 3141686 | doi = 10.1186/1743-422X-8-334 }}</ref> In normal cells, CDV activates caspase-8 first, which works as the initiator protein followed by the executioner protein caspase-3.<ref name=DelPuerto/> However, apoptosis induced by CDV in HeLa cells does not involve the initiator protein caspase-8. HeLa cell apoptosis caused by CDV follows a different mechanism than that in vero cell lines.<ref name=DelPuerto/> This change in the caspase cascade suggests CDV induces apoptosis via the [[intrinsic apoptosis|intrinsic pathway]], excluding the need for the initiator caspase-8. The executioner protein is instead activated by the internal stimuli caused by viral infection not a caspase cascade.<ref name=DelPuerto/> |
|||
The [[Oropouche virus]] (OROV) is found in the family ''[[Bunyaviridae]]''. The study of apoptosis brought on by ''Bunyaviridae'' was initiated in 1996, when it was observed that apoptosis was induced by the La Crosse virus into the kidney cells of baby hamsters and into the brains of baby mice.<ref name=Acrani>{{cite journal | vauthors = Acrani GO, Gomes R, Proença-Módena JL, da Silva AF, Carminati PO, Silva ML, Santos RI, Arruda E | title = Apoptosis induced by Oropouche virus infection in HeLa cells is dependent on virus protein expression | journal = Virus Research | volume = 149 | issue = 1 | pages = 56–63 | date = April 2010 | pmid = 20080135 | doi = 10.1016/j.virusres.2009.12.013 }}</ref> |
|||
OROV is a disease that is transmitted between humans by the biting midge (''[[Culicoides paraensis]]'').<ref name=Azevedo>{{cite journal | vauthors = Azevedo RS, Nunes MR, Chiang JO, Bensabath G, Vasconcelos HB, Pinto AY, Martins LC, Monteiro HA, Rodrigues SG, Vasconcelos PF | title = Reemergence of Oropouche fever, northern Brazil | journal = Emerging Infectious Diseases | volume = 13 | issue = 6 | pages = 912–15 | date = June 2007 | pmid = 17553235 | pmc = 2792853 | doi = 10.3201/eid1306.061114 }}</ref> It is referred to as a [[zoonotic]] [[arbovirus]] and causes febrile illness, characterized by the onset of a sudden fever known as Oropouche fever.<ref name=Santos>{{cite journal | vauthors = Santos RI, Rodrigues AH, Silva ML, Mortara RA, Rossi MA, Jamur MC, Oliver C, Arruda E | title = Oropouche virus entry into HeLa cells involves clathrin and requires endosomal acidification | journal = Virus Research | volume = 138 | issue = 1–2 | pages = 139–43 | date = December 2008 | pmid = 18840482 | doi = 10.1016/j.virusres.2008.08.016 | pmc = 7114418 }}</ref> |
|||
The Oropouche virus also causes disruption in cultured cells – cells that are cultivated in distinct and specific conditions. An example of this can be seen in [[HeLa cells]], whereby the cells begin to degenerate shortly after they are infected.<ref name=Acrani/> |
|||
With the use of [[gel electrophoresis]], it can be observed that OROV causes [[DNA]] fragmentation in HeLa cells. It can be interpreted by counting, measuring, and analyzing the cells of the Sub/G1 cell population.<ref name=Acrani/> When HeLA cells are infected with OROV, the [[cytochrome C]] is released from the membrane of the mitochondria, into the cytosol of the cells. This type of interaction shows that apoptosis is activated via an intrinsic pathway.<ref name=Indran/> |
|||
In order for apoptosis to occur within OROV, viral uncoating, viral internalization, along with the replication of cells is necessary. Apoptosis in some viruses is activated by extracellular stimuli. However, studies have demonstrated that the OROV infection causes apoptosis to be activated through intracellular stimuli and involves the mitochondria.<ref name=Acrani/> |
|||
Many viruses encode proteins that can inhibit apoptosis.<ref name=Teodora>{{cite journal | vauthors = Teodoro JG, Branton PE | title = Regulation of apoptosis by viral gene products | journal = Journal of Virology | volume = 71 | issue = 3 | pages = 1739–46 | date = March 1997 | pmid = 9032302 | pmc = 191242 | doi = 10.1128/jvi.71.3.1739-1746.1997 }}</ref> Several viruses encode viral homologs of Bcl-2. These homologs can inhibit proapoptotic proteins such as BAX and BAK, which are essential for the activation of apoptosis. Examples of viral Bcl-2 proteins include the [[Epstein-Barr virus]] BHRF1 protein and the [[adenovirus]] E1B 19K protein.<ref name=Polster>{{cite journal | vauthors = Polster BM, Pevsner J, Hardwick JM | title = Viral Bcl-2 homologs and their role in virus replication and associated diseases | journal = Biochimica et Biophysica Acta (BBA) - Molecular Cell Research | volume = 1644 | issue = 2–3 | pages = 211–27 | date = March 2004 | pmid = 14996505 | doi = 10.1016/j.bbamcr.2003.11.001 }}</ref> Some viruses express caspase inhibitors that inhibit caspase activity and an example is the CrmA protein of cowpox viruses. Whilst a number of viruses can block the effects of TNF and Fas. For example, the M-T2 protein of myxoma viruses can bind TNF preventing it from binding the TNF receptor and inducing a response.<ref name=Hay>{{cite journal | vauthors = Hay S, Kannourakis G | title = A time to kill: viral manipulation of the cell death program | journal = The Journal of General Virology | volume = 83 | issue = Pt 7 | pages = 1547–64 | date = July 2002 | pmid = 12075073 | doi = 10.1099/0022-1317-83-7-1547 | citeseerx = 10.1.1.322.6923 }}</ref> Furthermore, many viruses express p53 inhibitors that can bind p53 and inhibit its transcriptional transactivation activity. As a consequence, p53 cannot induce apoptosis, since it cannot induce the expression of proapoptotic proteins. The adenovirus E1B-55K protein and the [[hepatitis B virus]] HBx protein are examples of viral proteins that can perform such a function.<ref name=Wang>{{cite journal | vauthors = Wang XW, Gibson MK, Vermeulen W, Yeh H, Forrester K, Stürzbecher HW, Hoeijmakers JH, Harris CC | title = Abrogation of p53-induced apoptosis by the hepatitis B virus X gene | journal = Cancer Research | volume = 55 | issue = 24 | pages = 6012–16 | date = December 1995 | pmid = 8521383 }}</ref> |
|||
Viruses can remain intact from apoptosis in particular in the latter stages of infection. They can be exported in the ''apoptotic bodies'' that pinch off from the surface of the dying cell, and the fact that they are engulfed by phagocytes prevents the initiation of a host response. This favours the spread of the virus.<ref name="Hay"/> |
|||
==Plants== |
|||
[[Programmed cell death]] in plants has a number of molecular similarities to that of animal apoptosis, but it also has differences, notable ones being the presence of a [[cell wall]] and the lack of an [[immune system]] that removes the pieces of the dead cell. Instead of an immune response, the dying cell synthesizes substances to break itself down and places them in a [[vacuole]] that ruptures as the cell dies. Whether this whole process resembles animal apoptosis closely enough to warrant using the name ''apoptosis'' (as opposed to the more general ''programmed cell death'') is unclear.<ref>{{Cite journal | url = http://elfosscientiae.cigb.edu.cu/PDFs/BA/2006/23/1/BA002301RV001-010.pdf | title = Programmed cell death in plants resembles apoptosis of animals | first1 = Cyrelys | last1 = Collazo | first2 = Osmani | last2 = Chacón | first3 = Orlando | last3 = Borrás | name-list-style = vanc | journal = Biotecnología Aplicada | year = 2006 | volume = 23 | pages = 1–10 | url-status = dead | archive-url = https://web.archive.org/web/20090303235946/http://elfosscientiae.cigb.edu.cu/PDFs/BA/2006/23/1/BA002301RV001-010.pdf | archive-date = 2009-03-03 }}</ref><ref name=dickman2017>{{cite journal|doi=10.1038/s41477-017-0020-x|title=Reassessing apoptosis in plants|year=2017|last1=Dickman|first1=Martin|last2=Williams|first2=Brett|last3=Li|first3=Yurong|last4=De Figueiredo|first4=Paul|last5=Wolpert|first5=Thomas|journal=Nature Plants|volume=3|issue=10|pages=773–779|pmid=28947814|s2cid=3290201}}</ref> |
|||
==Caspase-independent apoptosis== |
|||
The characterization of the caspases allowed the development of caspase inhibitors, which can be used to determine whether a cellular process involves active caspases. Using these inhibitors it was discovered that cells can die while displaying a morphology similar to apoptosis without caspase activation.<ref name="pmid8962091">{{cite journal | vauthors = Xiang J, Chao DT, Korsmeyer SJ | title = BAX-induced cell death may not require interleukin 1 beta-converting enzyme-like proteases | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 93 | issue = 25 | pages = 14559–63 | date = December 1996 | pmid = 8962091 | pmc = 26172 | doi = 10.1073/pnas.93.25.14559 | bibcode = 1996PNAS...9314559X }}</ref> Later studies linked this phenomenon to the release of AIF ([[apoptosis-inducing factor]]) from the mitochondria and its translocation into the nucleus mediated by its NLS (nuclear localization signal). Inside the mitochondria, AIF is anchored to the inner membrane. In order to be released, the protein is cleaved by a calcium-dependent [[Calpain|calpain protease]]. |
|||
== See also == |
|||
{{Portal|Biology}} |
|||
{{div col|colwidth=22em}} |
|||
* [[Anoikis]] |
|||
* [[Apaf-1]] |
|||
* [[Apo2.7]] |
|||
* [[Apoptotic DNA fragmentation]] |
|||
* [[Atromentin]] induces apoptosis in human [[leukemia]] [[U937 cells]].<ref>{{cite journal|doi=10.4014/jmb.0811.617|pmid=19809251|title=Atromentin-Induced Apoptosis in Human Leukemia U937 Cells|journal=Journal of Microbiology and Biotechnology|volume=19|issue=9|pages=946–950|year=2009|last1=Kim|first1=Jin Hee|last2=Lee|first2=C. H.|s2cid=11552839}}</ref> |
|||
* [[Autolysis (biology)|Autolysis]] |
|||
* [[Autophagy]] |
|||
* [[Cisplatin]] |
|||
* [[Cytotoxicity]] |
|||
* [[Entosis]] |
|||
* [[Ferroptosis]] |
|||
* [[Homeostasis]] |
|||
* [[Immunology]] |
|||
* [[Necrobiosis]] |
|||
* [[Necrosis]] |
|||
* [[Necrotaxis]] |
|||
* [[Nemosis]] |
|||
* [[p53]] |
|||
* [[Paraptosis]] |
|||
* [[Pseudoapoptosis]] |
|||
* [[PI3K/AKT/mTOR pathway]] |
|||
{{div col end}} |
|||
== Explanatory footnotes == |
|||
{{notelist}} |
|||
== Citations == |
|||
{{Reflist|35em}} |
|||
== General bibliography == |
|||
{{Refbegin}} |
|||
* {{Cite book |last1=Alberts |first1=Bruce| last2=Johnson| first2=Alexander |last3=Lewis |first3=Julian |last4=Morgan |first4=David |last5=Raff |first5=Martin |last6=Roberts |first6=Keith |last7=Walter |first7=Peter | name-list-style = vanc |year=2015 |title=Molecular Biology of the Cell |edition=6th |publisher=Garland Science |page=2 |isbn=978-0815344322 |ref={{sfnRef|Alberts}}}} |
|||
{{Refend}} |
|||
== External links == |
|||
* [http://biovisi.com/APOPTOSIS_CASPASE3_VIDEO.php Apoptosis & cell surface]{{dead link|date=October 2016 |bot=InternetArchiveBot |fix-attempted=yes }} |
|||
* [https://www.youtube.com/watch?v=l4D0YxGi5Ec Apoptosis & Caspase 3], [[The Proteolysis Map]] – animation |
|||
* [https://www.youtube.com/watch?v=29AMumxsEo0 Apoptosis & Caspase 8], [[The Proteolysis Map]] – animation |
|||
* [https://www.youtube.com/watch?v=4YYboqiol_w Apoptosis & Caspase 7], [[The Proteolysis Map]] – animation |
|||
* [http://www.copewithcytokines.de/cope.cgi?key=Apoptosis%20MiniCOPE%20Dictionary Apoptosis MiniCOPE Dictionary – list of apoptosis terms and acronyms] |
|||
* [http://www.biochemweb.net/apoptosis.shtml Apoptosis (Programmed Cell Death) – The Virtual Library of Biochemistry, Molecular Biology and Cell Biology] |
|||
* [https://web.archive.org/web/20140825065034/http://www.caspases.org/ Apoptosis Research Portal] |
|||
* [https://web.archive.org/web/20070111132934/http://apoptosisinfo.com/ Apoptosis Info] Apoptosis protocols, articles, news, and recent publications. |
|||
* [https://web.archive.org/web/20070111190837/http://www.apoptosis-db.org/welcome.html Database of proteins involved in apoptosis] |
|||
* [https://web.archive.org/web/20070630103651/http://stke.sciencemag.org/content/vol2007/issue380/images/data/tr1/DC1/Apoptosis_WEHI.mov Apoptosis Video] |
|||
* [https://www.youtube.com/watch?v=DR80Huxp4y8 Apoptosis Video (WEHI on YouTube )] |
|||
* [http://users.rcn.com/jkimball.ma.ultranet/BiologyPages/A/Apoptosis.html#The_Mechanisms_of_Apoptosis The Mechanisms of Apoptosis] Kimball's Biology Pages. Simple explanation of the mechanisms of apoptosis triggered by internal signals (bcl-2), along the caspase-9, caspase-3 and caspase-7 pathway; and by external signals (FAS and TNF), along the caspase 8 pathway. Accessed 25 March 2007. |
|||
* WikiPathways – [http://www.wikipathways.org/index.php/Pathway:Homo_sapiens:Apoptosis Apoptosis pathway] |
|||
* [https://web.archive.org/web/20141227072014/http://www.crmagazine.org/archive/Spring2007/Pages/FindingCancersSelf-DestructButton.aspx "Finding Cancer's Self-Destruct Button"]. ''CR'' magazine (Spring 2007). Article on apoptosis and cancer. |
|||
* [http://www.ibiology.org/ibioseminars/cell-biology/xiaodong-wang-part-1.html Xiaodong Wang's lecture: Introduction to Apoptosis] |
|||
* [https://www.ibiology.org/cell-biology/programmed-cell-death/ Robert Horvitz's Short Clip: Discovering Programmed Cell Death] |
|||
* [http://bcl2db.ibcp.fr/BCL2DB/ The Bcl-2 Database] |
|||
* [http://arquivo.pt/wayback/20160515224643/http://www.deathbase.org/ DeathBase: a database of proteins involved in cell death, curated by experts] |
|||
* [http://www.ecdo.eu European Cell Death Organization] |
|||
* [https://www.cusabio.com/Apoptosis/ Apoptosis signaling pathway] created by Cusabio |
|||
{{Cell cycle proteins}} |
|||
{{Signal transduction}} |
|||
{{Apoptosis signaling pathway}} |
|||
{{Authority control}} |
|||
[[Category:Apoptosis| ]] |
|||
[[Category:Cell signaling]] |
|||
[[Category:Cellular senescence]] |
|||
[[Category:Immunology]] |
|||
[[Category:Medical aspects of death]] |
|||
[[Category:Programmed cell death]] |
|||
২০:০১, ৫ মার্চ ২০২১ তারিখে সংশোধিত সংস্করণ
এই নিবন্ধ থেকে {{Short description}} সরান। এটি বাংলা উইকিপিডিয়ায় কাজ করবে না।
| Apoptosis | |
|---|---|
 An etoposide-treated DU145 prostate cancer cell exploding into a cascade of apoptotic bodies. The sub images were extracted from a 61-hour time-lapse microscopy video, created using quantitative phase-contrast microscopy. The optical thickness is color-coded. With increasing thickness, color changes from gray to yellow, red, purple and finally black. See the video at The Cell: An Image Library | |
| শনাক্তকারী | |
| মে-এসএইচ | D017209 |
| শারীরস্থান পরিভাষা | |

Apoptosis (from Ancient Greek ἀπόπτωσις, apóptōsis, "falling off") is a form of programmed cell death that occurs in multicellular organisms.[১] Biochemical events lead to characteristic cell changes (morphology) and death. These changes include blebbing, cell shrinkage, nuclear fragmentation, chromatin condensation, chromosomal DNA fragmentation, and global[অস্পষ্ট] mRNA decay. The average adult human loses between 50 and 70 billion cells each day due to apoptosis.[ক] For an average human child between the ages of 8 and 14, approximately 20–30 billion cells die per day.[৩]
In contrast to necrosis, which is a form of traumatic cell death that results from acute cellular injury, apoptosis is a highly regulated and controlled process that confers advantages during an organism's life cycle. For example, the separation of fingers and toes in a developing human embryo occurs because cells between the digits undergo apoptosis. Unlike necrosis, apoptosis produces cell fragments called apoptotic bodies that phagocytic cells are able to engulf and remove before the contents of the cell can spill out onto surrounding cells and cause damage to them.[৪]
Because apoptosis cannot stop once it has begun, it is a highly regulated process. Apoptosis can be initiated through one of two pathways. In the intrinsic pathway the cell kills itself because it senses cell stress, while in the extrinsic pathway the cell kills itself because of signals from other cells. Weak external signals may also activate the intrinsic pathway of apoptosis.[৫] Both pathways induce cell death by activating caspases, which are proteases, or enzymes that degrade proteins. The two pathways both activate initiator caspases, which then activate executioner caspases, which then kill the cell by degrading proteins indiscriminately.
In addition to its importance as a biological phenomenon, defective apoptotic processes have been implicated in a wide variety of diseases. Excessive apoptosis causes atrophy, whereas an insufficient amount results in uncontrolled cell proliferation, such as cancer. Some factors like Fas receptors and caspases promote apoptosis, while some members of the Bcl-2 family of proteins inhibit apoptosis.
Discovery and etymology
German scientist Carl Vogt was first to describe the principle of apoptosis in 1842. In 1885, anatomist Walther Flemming delivered a more precise description of the process of programmed cell death. However, it was not until 1965 that the topic was resurrected. While studying tissues using electron microscopy, John Foxton Ross Kerr at the University of Queensland was able to distinguish apoptosis from traumatic cell death.[৬] Following the publication of a paper describing the phenomenon, Kerr was invited to join Alastair R. Currie, as well as Andrew Wyllie, who was Currie's graduate student,[৭] at University of Aberdeen. In 1972, the trio published a seminal article in the British Journal of Cancer.[৮] Kerr had initially used the term programmed cell necrosis, but in the article, the process of natural cell death was called apoptosis. Kerr, Wyllie and Currie credited James Cormack, a professor of Greek language at University of Aberdeen, with suggesting the term apoptosis. Kerr received the Paul Ehrlich and Ludwig Darmstaedter Prize on March 14, 2000, for his description of apoptosis. He shared the prize with Boston biologist H. Robert Horvitz.[৯]
For many years, neither "apoptosis" nor "programmed cell death" was a highly cited term. Two discoveries brought cell death from obscurity to a major field of research: identification of components of the cell death control and effector mechanisms, and linkage of abnormalities in cell death to human disease, in particular cancer.
The 2002 Nobel Prize in Medicine was awarded to Sydney Brenner, Horvitz and John E. Sulston for their work identifying genes that control apoptosis. The genes were identified by studies in the nematode C. elegans and homologues of these genes function in humans to regulate apoptosis.

In Greek, apoptosis translates to the "falling off" of leaves from a tree.[১০] Cormack, professor of Greek language, reintroduced the term for medical use as it had a medical meaning for the Greeks over two thousand years before. Hippocrates used the term to mean "the falling off of the bones". Galen extended its meaning to "the dropping of the scabs". Cormack was no doubt aware of this usage when he suggested the name. Debate continues over the correct pronunciation, with opinion divided between a pronunciation with the second p silent (/æpəˈtoʊsɪs/ ap-ə-TOH-sis[১১][১২]) and the second p pronounced (/eɪpəpˈtoʊsɪs/),[১১][১৩] as in the original Greek.[তথ্যসূত্র প্রয়োজন] In English, the p of the Greek -pt- consonant cluster is typically silent at the beginning of a word (e.g. pterodactyl, Ptolemy), but articulated when used in combining forms preceded by a vowel, as in helicopter or the orders of insects: diptera, lepidoptera, etc.
In the original Kerr, Wyllie & Currie paper,[৮] there is a footnote regarding the pronunciation:
We are most grateful to Professor James Cormack of the Department of Greek, University of Aberdeen, for suggesting this term. The word "apoptosis" (ἀπόπτωσις) is used in Greek to describe the "dropping off" or "falling off" of petals from flowers, or leaves from trees. To show the derivation clearly, we propose that the stress should be on the penultimate syllable, the second half of the word being pronounced like "ptosis" (with the "p" silent), which comes from the same root "to fall", and is already used to describe the drooping of the upper eyelid.
Activation mechanisms


The initiation of apoptosis is tightly regulated by activation mechanisms, because once apoptosis has begun, it inevitably leads to the death of the cell.[১৪][১৫] The two best-understood activation mechanisms are the intrinsic pathway (also called the mitochondrial pathway) and the extrinsic pathway.[১৬] The intrinsic pathway is activated by intracellular signals generated when cells are stressed and depends on the release of proteins from the intermembrane space of mitochondria.[১৭] The extrinsic pathway is activated by extracellular ligands binding to cell-surface death receptors, which leads to the formation of the death-inducing signaling complex (DISC).[১৮]
A cell initiates intracellular apoptotic signaling in response to a stress,[১৯] which may bring about cell suicide. The binding of nuclear receptors by glucocorticoids,[২০] heat,[২০] radiation,[২০] nutrient deprivation,[২০] viral infection,[২০] hypoxia,[২০] increased intracellular concentration of free fatty acids[২১] and increased intracellular calcium concentration,[২২][২৩] for example, by damage to the membrane, can all trigger the release of intracellular apoptotic signals by a damaged cell. A number of cellular components, such as poly ADP ribose polymerase, may also help regulate apoptosis.[২৪] Single cell fluctuations have been observed in experimental studies of stress induced apoptosis.[২৫][২৬]
Before the actual process of cell death is precipitated by enzymes, apoptotic signals must cause regulatory proteins to initiate the apoptosis pathway. This step allows those signals to cause cell death, or the process to be stopped, should the cell no longer need to die. Several proteins are involved, but two main methods of regulation have been identified: the targeting of mitochondria functionality,[২৭] or directly transducing the signal via adaptor proteins to the apoptotic mechanisms. An extrinsic pathway for initiation identified in several toxin studies is an increase in calcium concentration within a cell caused by drug activity, which also can cause apoptosis via a calcium binding protease calpain.
Intrinsic pathway
The intrinsic pathway is also known as the mitochondrial pathway. Mitochondria are essential to multicellular life. Without them, a cell ceases to respire aerobically and quickly dies. This fact forms the basis for some apoptotic pathways. Apoptotic proteins that target mitochondria affect them in different ways. They may cause mitochondrial swelling through the formation of membrane pores, or they may increase the permeability of the mitochondrial membrane and cause apoptotic effectors to leak out.[২০][২৮] They are very closely related to intrinsic pathway, and tumors arise more frequently through intrinsic pathway than the extrinsic pathway because of sensitivity.[২৯] There is also a growing body of evidence indicating that nitric oxide is able to induce apoptosis by helping to dissipate the membrane potential of mitochondria and therefore make it more permeable.[৩০] Nitric oxide has been implicated in initiating and inhibiting apoptosis through its possible action as a signal molecule of subsequent pathways that activate apoptosis.[৩১]
During apoptosis, cytochrome c is released from mitochondria through the actions of the proteins Bax and Bak. The mechanism of this release is enigmatic, but appears to stem from a multitude of Bax/Bak homo- and hetero-dimers of Bax/Bak inserted into the outer membrane.[৩২] Once cytochrome c is released it binds with Apoptotic protease activating factor – 1 (Apaf-1) and ATP, which then bind to pro-caspase-9 to create a protein complex known as an apoptosome. The apoptosome cleaves the pro-caspase to its active form of caspase-9, which in turn cleaves and activates pro-caspase into the effector caspase-3.
Mitochondria also release proteins known as SMACs (second mitochondria-derived activator of caspases) into the cell's cytosol following the increase in permeability of the mitochondria membranes. SMAC binds to proteins that inhibit apoptosis (IAPs) thereby deactivating them, and preventing the IAPs from arresting the process and therefore allowing apoptosis to proceed. IAP also normally suppresses the activity of a group of cysteine proteases called caspases,[৩৩] which carry out the degradation of the cell. Therefore, the actual degradation enzymes can be seen to be indirectly regulated by mitochondrial permeability.
Extrinsic pathway
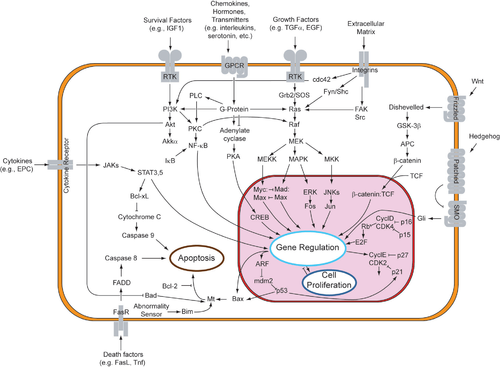
Two theories of the direct initiation of apoptotic mechanisms in mammals have been suggested: the TNF-induced (tumor necrosis factor) model and the Fas-Fas ligand-mediated model, both involving receptors of the TNF receptor (TNFR) family[৩৪] coupled to extrinsic signals.
TNF path
TNF-alpha is a cytokine produced mainly by activated macrophages, and is the major extrinsic mediator of apoptosis. Most cells in the human body have two receptors for TNF-alpha: TNFR1 and TNFR2. The binding of TNF-alpha to TNFR1 has been shown to initiate the pathway that leads to caspase activation via the intermediate membrane proteins TNF receptor-associated death domain (TRADD) and Fas-associated death domain protein (FADD). cIAP1/2 can inhibit TNF-α signaling by binding to TRAF2. FLIP inhibits the activation of caspase-8.[৩৫] Binding of this receptor can also indirectly lead to the activation of transcription factors involved in cell survival and inflammatory responses.[৩৬] However, signalling through TNFR1 might also induce apoptosis in a caspase-independent manner.[৩৭] The link between TNF-alpha and apoptosis shows why an abnormal production of TNF-alpha plays a fundamental role in several human diseases, especially in autoimmune diseases. The TNF-alpha receptor superfamily also includes death receptors (DRs), such as DR4 and DR5. These receptors bind to the proteinTRAIL and mediate apoptosis. Apoptosis is known to be one of the primary mechanisms of targeted cancer therapy.[৩৮] Luminescent iridium complex-peptide hybrids (IPHs) have recently been designed, which mimic TRAIL and bind to death receptors on cancer cells, thereby inducing their apoptosis.[৩৯]
- Fas path
The fas receptor (First apoptosis signal) – (also known as Apo-1 or CD95) is a transmembrane protein of the TNF family which binds the Fas ligand (FasL).[৩৪] The interaction between Fas and FasL results in the formation of the death-inducing signaling complex (DISC), which contains the FADD, caspase-8 and caspase-10. In some types of cells (type I), processed caspase-8 directly activates other members of the caspase family, and triggers the execution of apoptosis of the cell. In other types of cells (type II), the Fas-DISC starts a feedback loop that spirals into increasing release of proapoptotic factors from mitochondria and the amplified activation of caspase-8.[৪০]
- Common components
Following TNF-R1 and Fas activation in mammalian cells[তথ্যসূত্র প্রয়োজন] a balance between proapoptotic (BAX,[৪১] BID, BAK, or BAD) and anti-apoptotic (Bcl-Xl and Bcl-2) members of the Bcl-2 family are established. This balance is the proportion of proapoptotic homodimers that form in the outer-membrane of the mitochondrion. The proapoptotic homodimers are required to make the mitochondrial membrane permeable for the release of caspase activators such as cytochrome c and SMAC. Control of proapoptotic proteins under normal cell conditions of nonapoptotic cells is incompletely understood, but in general, Bax or Bak are activated by the activation of BH3-only proteins, part of the Bcl-2 family[তথ্যসূত্র প্রয়োজন].
- Caspases
Caspases play the central role in the transduction of ER apoptotic signals. Caspases are proteins that are highly conserved, cysteine-dependent aspartate-specific proteases. There are two types of caspases: initiator caspases, caspase 2,8,9,10,11,12, and effector caspases, caspase 3,6,7. The activation of initiator caspases requires binding to specific oligomeric activator protein. Effector caspases are then activated by these active initiator caspases through proteolytic cleavage. The active effector caspases then proteolytically degrade a host of intracellular proteins to carry out the cell death program.
- Caspase-independent apoptotic pathway
There also exists a caspase-independent apoptotic pathway that is mediated by AIF (apoptosis-inducing factor).[৪২]
Apoptosis model in amphibians
Amphibian frog Xenopus laevis serves as an ideal model system for the study of the mechanisms of apoptosis. In fact, iodine and thyroxine also stimulate the spectacular apoptosis of the cells of the larval gills, tail and fins in amphibians metamorphosis, and stimulate the evolution of their nervous system transforming the aquatic, vegetarian tadpole into the terrestrial, carnivorous frog.[৪৩][৪৪][৪৫][৪৬]
Negative regulators of apoptosis
Negative regulation of apoptosis inhibits cell death signaling pathways, helping tumors to evade cell death and developing drug resistance. The ratio between anti-apoptotic (Bcl-2) and pro-apoptotic (Bax) proteins determines whether a cell lives or dies.[৪৭][৪৮] Many families of proteins act as negative regulators categorized into either antiapoptotic factors, such as IAPs and Bcl-2 proteins or prosurvival factors like cFLIP, BNIP3, FADD, Akt, and NF-κB.[৪৯]
Proteolytic caspase cascade: Killing the cell
Many pathways and signals lead to apoptosis, but these converge on a single mechanism that actually causes the death of the cell. After a cell receives stimulus, it undergoes organized degradation of cellular organelles by activated proteolytic caspases. In addition to the destruction of cellular organelles, mRNA is rapidly and globally degraded by a mechanism that is not yet fully characterized.[৫০] mRNA decay is triggered very early in apoptosis.
A cell undergoing apoptosis shows a series of characteristic morphological changes. Early alterations include:
- Cell shrinkage and rounding occur because of the retraction lamellipodia and the breakdown of the proteinaceous cytoskeleton by caspases.[৫১]
- The cytoplasm appears dense, and the organelles appear tightly packed.
- Chromatin undergoes condensation into compact patches against the nuclear envelope (also known as the perinuclear envelope) in a process known as pyknosis, a hallmark of apoptosis.[৫২][৫৩]
- The nuclear envelope becomes discontinuous and the DNA inside it is fragmented in a process referred to as karyorrhexis. The nucleus breaks into several discrete chromatin bodies or nucleosomal units due to the degradation of DNA.[৫৪]
Apoptosis progresses quickly and its products are quickly removed, making it difficult to detect or visualize on classical histology sections. During karyorrhexis, endonuclease activation leaves short DNA fragments, regularly spaced in size. These give a characteristic "laddered" appearance on agar gel after electrophoresis.[৫৫] Tests for DNA laddering differentiate apoptosis from ischemic or toxic cell death.[৫৬]
Apoptotic cell disassembly

Before the apoptotic cell is disposed of, there is a process of disassembly. There are three recognized steps in apoptotic cell disassembly:[৫৮]
- Membrane blebbing: The cell membrane shows irregular buds known as blebs. Initially these are smaller surface blebs. Later these can grow into larger so-called dynamic membrane blebs.[৫৮] An important regulator of apoptotic cell membrane blebbing is ROCK1 (rho associated coiled-coil-containing protein kinase 1).[৫৯][৬০]
- Formation of membrane protrusions: Some cell types, under specific conditions, may develop different types of long, thin extensions of the cell membrane called membrane protrusions. Three types have been described: microtubule spikes, apoptopodia (feet of death), and beaded apoptopodia (the latter having a beads-on-a-string appearance).[৬১][৬২][৬৩] Pannexin 1 is an important component of membrane channels involved in the formation of apoptopodia and beaded apoptopodia.[৬২]
- Fragmentation: The cell breaks apart into multiple vesicles called apoptotic bodies, which undergo phagocytosis. The plasma membrane protrusions may help bring apoptotic bodies closer to phagocytes.
Removal of dead cells
The removal of dead cells by neighboring phagocytic cells has been termed efferocytosis.[৬৪] Dying cells that undergo the final stages of apoptosis display phagocytotic molecules, such as phosphatidylserine, on their cell surface.[৬৫] Phosphatidylserine is normally found on the inner leaflet surface of the plasma membrane, but is redistributed during apoptosis to the extracellular surface by a protein known as scramblase.[৬৬] These molecules mark the cell for phagocytosis by cells possessing the appropriate receptors, such as macrophages.[৬৭] The removal of dying cells by phagocytes occurs in an orderly manner without eliciting an inflammatory response.[৬৮] During apoptosis cellular RNA and DNA are separated from each other and sorted to different apoptotic bodies; separation of RNA is initiated as nucleolar segregation.[৬৯]
Pathway knock-outs
Many knock-outs have been made in the apoptosis pathways to test the function of each of the proteins. Several caspases, in addition to APAF1 and FADD, have been mutated to determine the new phenotype. In order to create a tumor necrosis factor (TNF) knockout, an exon containing the nucleotides 3704–5364 was removed from the gene. This exon encodes a portion of the mature TNF domain, as well as the leader sequence, which is a highly conserved region necessary for proper intracellular processing. TNF-/- mice develop normally and have no gross structural or morphological abnormalities. However, upon immunization with SRBC (sheep red blood cells), these mice demonstrated a deficiency in the maturation of an antibody response; they were able to generate normal levels of IgM, but could not develop specific IgG levels. Apaf-1 is the protein that turns on caspase 9 by cleavage to begin the caspase cascade that leads to apoptosis. Since a -/- mutation in the APAF-1 gene is embryonic lethal, a gene trap strategy was used in order to generate an APAF-1 -/- mouse. This assay is used to disrupt gene function by creating an intragenic gene fusion. When an APAF-1 gene trap is introduced into cells, many morphological changes occur, such as spina bifida, the persistence of interdigital webs, and open brain. In addition, after embryonic day 12.5, the brain of the embryos showed several structural changes. APAF-1 cells are protected from apoptosis stimuli such as irradiation. A BAX-1 knock-out mouse exhibits normal forebrain formation and a decreased programmed cell death in some neuronal populations and in the spinal cord, leading to an increase in motor neurons.
The caspase proteins are integral parts of the apoptosis pathway, so it follows that knock-outs made have varying damaging results. A caspase 9 knock-out leads to a severe brain malformation. A caspase 8 knock-out leads to cardiac failure and thus embryonic lethality. However, with the use of cre-lox technology, a caspase 8 knock-out has been created that exhibits an increase in peripheral T cells, an impaired T cell response, and a defect in neural tube closure. These mice were found to be resistant to apoptosis mediated by CD95, TNFR, etc. but not resistant to apoptosis caused by UV irradiation, chemotherapeutic drugs, and other stimuli. Finally, a caspase 3 knock-out was characterized by ectopic cell masses in the brain and abnormal apoptotic features such as membrane blebbing or nuclear fragmentation. A remarkable feature of these KO mice is that they have a very restricted phenotype: Casp3, 9, APAF-1 KO mice have deformations of neural tissue and FADD and Casp 8 KO showed defective heart development, however, in both types of KO other organs developed normally and some cell types were still sensitive to apoptotic stimuli suggesting that unknown proapoptotic pathways exist.
Methods for distinguishing apoptotic from necrotic (necroptotic) cells

In order to perform analysis of apoptotic versus necrotic (necroptotic) cells, one can do analysis of morphology by label-free live cell imaging, time-lapse microscopy, flow fluorocytometry, and transmission electron microscopy. There are also various biochemical techniques for analysis of cell surface markers (phosphatidylserine exposure versus cell permeability by flow cytometry), cellular markers such as DNA fragmentation[৭০] (flow cytometry),[৭১] caspase activation, Bid cleavage, and cytochrome c release (Western blotting). It is important to know how primary and secondary necrotic cells can be distinguished by analysis of supernatant for caspases, HMGB1, and release of cytokeratin 18. However, no distinct surface or biochemical markers of necrotic cell death have been identified yet, and only negative markers are available. These include absence of apoptotic markers (caspase activation, cytochrome c release, and oligonucleosomal DNA fragmentation) and differential kinetics of cell death markers (phosphatidylserine exposure and cell membrane permeabilization). A selection of techniques that can be used to distinguish apoptosis from necroptotic cells could be found in these references.[৭২][৭৩][৭৪][৭৫]
Implication in disease



Defective pathways
The many different types of apoptotic pathways contain a multitude of different biochemical components, many of them not yet understood.[৭৬] As a pathway is more or less sequential in nature, removing or modifying one component leads to an effect in another. In a living organism, this can have disastrous effects, often in the form of disease or disorder. A discussion of every disease caused by modification of the various apoptotic pathways would be impractical, but the concept overlying each one is the same: The normal functioning of the pathway has been disrupted in such a way as to impair the ability of the cell to undergo normal apoptosis. This results in a cell that lives past its "use-by date" and is able to replicate and pass on any faulty machinery to its progeny, increasing the likelihood of the cell's becoming cancerous or diseased.
A recently described example of this concept in action can be seen in the development of a lung cancer called NCI-H460.[৭৭] The X-linked inhibitor of apoptosis protein (XIAP) is overexpressed in cells of the H460 cell line. XIAPs bind to the processed form of caspase-9, and suppress the activity of apoptotic activator cytochrome c, therefore overexpression leads to a decrease in the amount of proapoptotic agonists. As a consequence, the balance of anti-apoptotic and proapoptotic effectors is upset in favour of the former, and the damaged cells continue to replicate despite being directed to die. Defects in regulation of apoptosis in cancer cells occur often at the level of control of transcription factors. As a particular example, defects in molecules that control transcription factor NF-κB in cancer change the mode of transcriptional regulation and the response to apoptotic signals, to curtail dependence on the tissue that the cell belongs. This degree of independence from external survival signals, can enable cancer metastasis.[৭৮]
Dysregulation of p53
The tumor-suppressor protein p53 accumulates when DNA is damaged due to a chain of biochemical factors. Part of this pathway includes alpha-interferon and beta-interferon, which induce transcription of the p53 gene, resulting in the increase of p53 protein level and enhancement of cancer cell-apoptosis.[৭৯] p53 prevents the cell from replicating by stopping the cell cycle at G1, or interphase, to give the cell time to repair, however it will induce apoptosis if damage is extensive and repair efforts fail.[৮০] Any disruption to the regulation of the p53 or interferon genes will result in impaired apoptosis and the possible formation of tumors.
Inhibition
Inhibition of apoptosis can result in a number of cancers, inflammatory diseases, and viral infections. It was originally believed that the associated accumulation of cells was due to an increase in cellular proliferation, but it is now known that it is also due to a decrease in cell death. The most common of these diseases is cancer, the disease of excessive cellular proliferation, which is often characterized by an overexpression of IAP family members. As a result, the malignant cells experience an abnormal response to apoptosis induction: Cycle-regulating genes (such as p53, ras or c-myc) are mutated or inactivated in diseased cells, and further genes (such as bcl-2) also modify their expression in tumors. Some apoptotic factors are vital during mitochondrial respiration e.g. cytochrome C.[৮১] Pathological inactivation of apoptosis in cancer cells is correlated with frequent respiratory metabolic shifts toward glycolysis (an observation known as the “Warburg hypothesis”.[৮২]
HeLa cell
Apoptosis in HeLa[খ] cells is inhibited by proteins produced by the cell; these inhibitory proteins target retinoblastoma tumor-suppressing proteins.[৮৩] These tumor-suppressing proteins regulate the cell cycle, but are rendered inactive when bound to an inhibitory protein.[৮৩] HPV E6 and E7 are inhibitory proteins expressed by the human papillomavirus, HPV being responsible for the formation of the cervical tumor from which HeLa cells are derived.[৮৪] HPV E6 causes p53, which regulates the cell cycle, to become inactive.[৮৫] HPV E7 binds to retinoblastoma tumor suppressing proteins and limits its ability to control cell division.[৮৫] These two inhibitory proteins are partially responsible for HeLa cells' immortality by inhibiting apoptosis to occur.[৮৬] CDV (Canine Distemper Virus) is able to induce apoptosis despite the presence of these inhibitory proteins. This is an important oncolytic property of CDV: this virus is capable of killing canine lymphoma cells. Oncoproteins E6 and E7 still leave p53 inactive, but they are not able to avoid the activation of caspases induced from the stress of viral infection. These oncolytic properties provided a promising link between CDV and lymphoma apoptosis, which can lead to development of alternative treatment methods for both canine lymphoma and human non-Hodgkin lymphoma. Defects in the cell cycle are thought to be responsible for the resistance to chemotherapy or radiation by certain tumor cells, so a virus that can induce apoptosis despite defects in the cell cycle is useful for cancer treatment.[৮৬]
Treatments
The main method of treatment for potential death from signaling-related diseases involves either increasing or decreasing the susceptibility of apoptosis in diseased cells, depending on whether the disease is caused by either the inhibition of or excess apoptosis. For instance, treatments aim to restore apoptosis to treat diseases with deficient cell death, and to increase the apoptotic threshold to treat diseases involved with excessive cell death. To stimulate apoptosis, one can increase the number of death receptor ligands (such as TNF or TRAIL), antagonize the anti-apoptotic Bcl-2 pathway, or introduce Smac mimetics to inhibit the inhibitor (IAPs).[৪৭] The addition of agents such as Herceptin, Iressa, or Gleevec works to stop cells from cycling and causes apoptosis activation by blocking growth and survival signaling further upstream. Finally, adding p53-MDM2 complexes displaces p53 and activates the p53 pathway, leading to cell cycle arrest and apoptosis. Many different methods can be used either to stimulate or to inhibit apoptosis in various places along the death signaling pathway.[৮৭]
Apoptosis is a multi-step, multi-pathway cell-death programme that is inherent in every cell of the body. In cancer, the apoptosis cell-division ratio is altered. Cancer treatment by chemotherapy and irradiation kills target cells primarily by inducing apoptosis.
Hyperactive apoptosis
On the other hand, loss of control of cell death (resulting in excess apoptosis) can lead to neurodegenerative diseases, hematologic diseases, and tissue damage. It is of interest to note that neurons that rely on mitochondrial respiration undergo apoptosis in neurodegenerative diseases such as Alzheimer's[৮৮] and Parkinson's.[৮৯] (an observation known as the “Inverse Warburg hypothesis” [৯০][৮১] ). Moreover, there is an inverse epidemiological comorbidity between neurodegenerative diseases and cancer.[৯১] The progression of HIV is directly linked to excess, unregulated apoptosis. In a healthy individual, the number of CD4+ lymphocytes is in balance with the cells generated by the bone marrow; however, in HIV-positive patients, this balance is lost due to an inability of the bone marrow to regenerate CD4+ cells. In the case of HIV, CD4+ lymphocytes die at an accelerated rate through uncontrolled apoptosis, when stimulated. At the molecular level, hyperactive apoptosis can be caused by defects in signaling pathways that regulate the Bcl-2 family proteins. Increased expression of apoptotic proteins such as BIM, or their decreased proteolysis, leads to cell death, and can cause a number of pathologies, depending on the cells where excessive activity of BIM occurs. Cancer cells can escape apoptosis through mechanisms that suppress BIM expression or by increased proteolysis of BIM.[তথ্যসূত্র প্রয়োজন]
Treatments
Treatments aiming to inhibit works to block specific caspases. Finally, the Akt protein kinase promotes cell survival through two pathways. Akt phosphorylates and inhibits Bad (a Bcl-2 family member), causing Bad to interact with the 14-3-3 scaffold, resulting in Bcl dissociation and thus cell survival. Akt also activates IKKα, which leads to NF-κB activation and cell survival. Active NF-κB induces the expression of anti-apoptotic genes such as Bcl-2, resulting in inhibition of apoptosis. NF-κB has been found to play both an antiapoptotic role and a proapoptotic role depending on the stimuli utilized and the cell type.[৯২]
HIV progression
The progression of the human immunodeficiency virus infection into AIDS is due primarily to the depletion of CD4+ T-helper lymphocytes in a manner that is too rapid for the body's bone marrow to replenish the cells, leading to a compromised immune system. One of the mechanisms by which T-helper cells are depleted is apoptosis, which results from a series of biochemical pathways:[৯৩]
- HIV enzymes deactivate anti-apoptotic Bcl-2. This does not directly cause cell death but primes the cell for apoptosis should the appropriate signal be received. In parallel, these enzymes activate proapoptotic procaspase-8, which does directly activate the mitochondrial events of apoptosis.
- HIV may increase the level of cellular proteins that prompt Fas-mediated apoptosis.
- HIV proteins decrease the amount of CD4 glycoprotein marker present on the cell membrane.
- Released viral particles and proteins present in extracellular fluid are able to induce apoptosis in nearby "bystander" T helper cells.
- HIV decreases the production of molecules involved in marking the cell for apoptosis, giving the virus time to replicate and continue releasing apoptotic agents and virions into the surrounding tissue.
- The infected CD4+ cell may also receive the death signal from a cytotoxic T cell.
Cells may also die as direct consequences of viral infections. HIV-1 expression induces tubular cell G2/M arrest and apoptosis.[৯৪] The progression from HIV to AIDS is not immediate or even necessarily rapid; HIV's cytotoxic activity toward CD4+ lymphocytes is classified as AIDS once a given patient's CD4+ cell count falls below 200.[৯৫]
Researchers from Kumamoto University in Japan have developed a new method to eradicate HIV in viral reservoir cells, named "Lock-in and apoptosis." Using the synthesized compound Heptanoylphosphatidyl L-Inositol Pentakisphophate (or L-Hippo) to bind strongly to the HIV protein PR55Gag, they were able to suppress viral budding. By suppressing viral budding, the researchers were able to trap the HIV virus in the cell and allow for the cell to undergo apoptosis (natural cell death). Associate Professor Mikako Fujita has stated that the approach is not yet available to HIV patients because the research team has to conduct further research on combining the drug therapy that currently exists with this "Lock-in and apoptosis" approach to lead to complete recovery from HIV.[৯৬]
Viral infection
Viral induction of apoptosis occurs when one or several cells of a living organism are infected with a virus, leading to cell death. Cell death in organisms is necessary for the normal development of cells and the cell cycle maturation.[৯৭] It is also important in maintaining the regular functions and activities of cells.
Viruses can trigger apoptosis of infected cells via a range of mechanisms including:
- Receptor binding
- Activation of protein kinase R (PKR)
- Interaction with p53
- Expression of viral proteins coupled to MHC proteins on the surface of the infected cell, allowing recognition by cells of the immune system (such as Natural Killer and cytotoxic T cells) that then induce the infected cell to undergo apoptosis.[৯৮]
Canine distemper virus (CDV) is known to cause apoptosis in central nervous system and lymphoid tissue of infected dogs in vivo and in vitro.[৯৯] Apoptosis caused by CDV is typically induced via the extrinsic pathway, which activates caspases that disrupt cellular function and eventually leads to the cells death.[৮৩] In normal cells, CDV activates caspase-8 first, which works as the initiator protein followed by the executioner protein caspase-3.[৮৩] However, apoptosis induced by CDV in HeLa cells does not involve the initiator protein caspase-8. HeLa cell apoptosis caused by CDV follows a different mechanism than that in vero cell lines.[৮৩] This change in the caspase cascade suggests CDV induces apoptosis via the intrinsic pathway, excluding the need for the initiator caspase-8. The executioner protein is instead activated by the internal stimuli caused by viral infection not a caspase cascade.[৮৩]
The Oropouche virus (OROV) is found in the family Bunyaviridae. The study of apoptosis brought on by Bunyaviridae was initiated in 1996, when it was observed that apoptosis was induced by the La Crosse virus into the kidney cells of baby hamsters and into the brains of baby mice.[১০০]
OROV is a disease that is transmitted between humans by the biting midge (Culicoides paraensis).[১০১] It is referred to as a zoonotic arbovirus and causes febrile illness, characterized by the onset of a sudden fever known as Oropouche fever.[১০২]
The Oropouche virus also causes disruption in cultured cells – cells that are cultivated in distinct and specific conditions. An example of this can be seen in HeLa cells, whereby the cells begin to degenerate shortly after they are infected.[১০০]
With the use of gel electrophoresis, it can be observed that OROV causes DNA fragmentation in HeLa cells. It can be interpreted by counting, measuring, and analyzing the cells of the Sub/G1 cell population.[১০০] When HeLA cells are infected with OROV, the cytochrome C is released from the membrane of the mitochondria, into the cytosol of the cells. This type of interaction shows that apoptosis is activated via an intrinsic pathway.[৯৭]
In order for apoptosis to occur within OROV, viral uncoating, viral internalization, along with the replication of cells is necessary. Apoptosis in some viruses is activated by extracellular stimuli. However, studies have demonstrated that the OROV infection causes apoptosis to be activated through intracellular stimuli and involves the mitochondria.[১০০]
Many viruses encode proteins that can inhibit apoptosis.[১০৩] Several viruses encode viral homologs of Bcl-2. These homologs can inhibit proapoptotic proteins such as BAX and BAK, which are essential for the activation of apoptosis. Examples of viral Bcl-2 proteins include the Epstein-Barr virus BHRF1 protein and the adenovirus E1B 19K protein.[১০৪] Some viruses express caspase inhibitors that inhibit caspase activity and an example is the CrmA protein of cowpox viruses. Whilst a number of viruses can block the effects of TNF and Fas. For example, the M-T2 protein of myxoma viruses can bind TNF preventing it from binding the TNF receptor and inducing a response.[১০৫] Furthermore, many viruses express p53 inhibitors that can bind p53 and inhibit its transcriptional transactivation activity. As a consequence, p53 cannot induce apoptosis, since it cannot induce the expression of proapoptotic proteins. The adenovirus E1B-55K protein and the hepatitis B virus HBx protein are examples of viral proteins that can perform such a function.[১০৬]
Viruses can remain intact from apoptosis in particular in the latter stages of infection. They can be exported in the apoptotic bodies that pinch off from the surface of the dying cell, and the fact that they are engulfed by phagocytes prevents the initiation of a host response. This favours the spread of the virus.[১০৫]
Plants
Programmed cell death in plants has a number of molecular similarities to that of animal apoptosis, but it also has differences, notable ones being the presence of a cell wall and the lack of an immune system that removes the pieces of the dead cell. Instead of an immune response, the dying cell synthesizes substances to break itself down and places them in a vacuole that ruptures as the cell dies. Whether this whole process resembles animal apoptosis closely enough to warrant using the name apoptosis (as opposed to the more general programmed cell death) is unclear.[১০৭][১০৮]
Caspase-independent apoptosis
The characterization of the caspases allowed the development of caspase inhibitors, which can be used to determine whether a cellular process involves active caspases. Using these inhibitors it was discovered that cells can die while displaying a morphology similar to apoptosis without caspase activation.[১০৯] Later studies linked this phenomenon to the release of AIF (apoptosis-inducing factor) from the mitochondria and its translocation into the nucleus mediated by its NLS (nuclear localization signal). Inside the mitochondria, AIF is anchored to the inner membrane. In order to be released, the protein is cleaved by a calcium-dependent calpain protease.
See also
Explanatory footnotes
- ↑ Note that the average human adult has more than 13 trillion cells (১.৩×১০১৩),[২] of which at most only 70 billion (৭.০×১০১০) die per day. That is, about 5 out of every 1,000 cells (0.5%) die each day due to apoptosis.
- ↑ HeLa cells are an immortalized cancer cell line used frequently in research. The cell line was established by removing cells directly from Henrietta Lacks, a cancer patient.
Citations
- ↑ Green, Douglas (২০১১)। Means to an End: Apoptosis and other Cell Death Mechanisms। Cold Spring Harbor, NY: Cold Spring Harbor Laboratory Press। আইএসবিএন 978-0-87969-888-1। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ Alberts, পৃ. 2।
- ↑ Karam, Jose A. (২০০৯)। Apoptosis in Carcinogenesis and Chemotherapy। Netherlands: Springer। আইএসবিএন 978-1-4020-9597-9। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ Alberts, Bruce; Johnson, Alexander; Lewis, Julian; Raff, Martin; Roberts, Keith; Walter, Peter (২০০৮)। "Chapter 18 Apoptosis: Programmed Cell Death Eliminates Unwanted Cells"। Molecular Biology of the Cell (textbook) (5th সংস্করণ)। Garland Science। পৃষ্ঠা 1115। আইএসবিএন 978-0-8153-4105-5। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ Raychaudhuri S (আগস্ট ২০১০)। "A minimal model of signaling network elucidates cell-to-cell stochastic variability in apoptosis"। PLOS ONE। 5 (8): e11930। arXiv:1009.2294
 । ডিওআই:10.1371/journal.pone.0011930। পিএমআইডি 20711445। পিএমসি 2920308
। ডিওআই:10.1371/journal.pone.0011930। পিএমআইডি 20711445। পিএমসি 2920308  । বিবকোড:2010PLoSO...511930R।
। বিবকোড:2010PLoSO...511930R।
- ↑ Kerr JF (অক্টোবর ১৯৬৫)। "A histochemical study of hypertrophy and ischaemic injury of rat liver with special reference to changes in lysosomes"। The Journal of Pathology and Bacteriology। 90 (2): 419–35। ডিওআই:10.1002/path.1700900210। পিএমআইডি 5849603।
- ↑ Agency for Science, Technology and Research। "Prof Andrew H. Wyllie – Lecture Abstract"। ২০০৭-১১-১৩ তারিখে মূল থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০০৭-০৩-৩০।
- ↑ ক খ Kerr JF, Wyllie AH, Currie AR (আগস্ট ১৯৭২)। "Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics"। British Journal of Cancer। 26 (4): 239–57। ডিওআই:10.1038/bjc.1972.33। পিএমআইডি 4561027। পিএমসি 2008650
 ।
।
- ↑ O'Rourke MG, Ellem KA (২০০০)। "John Kerr and apoptosis"। The Medical Journal of Australia। 173 (11–12): 616–17। এসটুসিআইডি 38265127। ডিওআই:10.5694/j.1326-5377.2000.tb139362.x। পিএমআইডি 11379508।
- ↑ Alberts, পৃ. 1021।
- ↑ ক খ American Heritage Dictionary ওয়েব্যাক মেশিনে আর্কাইভকৃত জুন ৩০, ২০০৮ তারিখে
- ↑ Apoptosis Interest Group (১৯৯৯)। "About apoptosis"। ২৮ ডিসেম্বর ২০০৬ তারিখে মূল থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০০৬-১২-১৫।
- ↑ "Definition of APOPTOSIS"। www.webster.com। ২০০৭-০৭-০৩ তারিখে মূল থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০০৭-০৮-১১।
- ↑ Alberts, পৃ. 1029।
- ↑ Böhm I, Schild H (২০০৩)। "Apoptosis: the complex scenario for a silent cell death"। Molecular Imaging and Biology। 5 (1): 2–14। ডিওআই:10.1016/S1536-1632(03)00024-6। পিএমআইডি 14499155।
- ↑ Alberts, পৃ. 1023।
- ↑ Alberts, পৃ. 1032।
- ↑ Alberts, পৃ. 1024।
- ↑ Nirmala GJ and Lopus M (2020) Cell death mechanisms in eukaryotes. Cell Biol Toxicol, 36, 145–164. doi: /10.1007/s10565-019-09496-2. PubMed
- ↑ ক খ গ ঘ ঙ চ ছ Cotran, Ramzi S.; Kumar, Collins (১৯৯৮)। Robbins Pathologic Basis of Disease। Philadelphia: W.B Saunders Company। আইএসবিএন 978-0-7216-7335-6। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ Hardy S, El-Assaad W, Przybytkowski E, Joly E, Prentki M, Langelier Y (আগস্ট ২০০৩)। "Saturated fatty acid-induced apoptosis in MDA-MB-231 breast cancer cells. A role for cardiolipin"। The Journal of Biological Chemistry। 278 (34): 31861–70। ডিওআই:10.1074/jbc.m300190200
 । পিএমআইডি 12805375।
। পিএমআইডি 12805375।
- ↑ Mattson MP, Chan SL (ডিসেম্বর ২০০৩)। "Calcium orchestrates apoptosis"। Nature Cell Biology। 5 (12): 1041–43। এসটুসিআইডি 38427579। ডিওআই:10.1038/ncb1203-1041। পিএমআইডি 14647298।
- ↑ Uğuz AC, Naziroğlu M, Espino J, Bejarano I, González D, Rodríguez AB, Pariente JA (ডিসেম্বর ২০০৯)। "Selenium modulates oxidative stress-induced cell apoptosis in human myeloid HL-60 cells through regulation of calcium release and caspase-3 and -9 activities"। The Journal of Membrane Biology। 232 (1–3): 15–23। এসটুসিআইডি 22215706। ডিওআই:10.1007/s00232-009-9212-2। পিএমআইডি 19898892।
- ↑ Chiarugi A, Moskowitz MA (জুলাই ২০০২)। "Cell biology. PARP-1 – a perpetrator of apoptotic cell death?"। Science। 297 (5579): 200–01। এসটুসিআইডি 82828773। ডিওআই:10.1126/science.1074592। পিএমআইডি 12114611।
- ↑ Goldstein JC, Waterhouse NJ, Juin P, Evan GI, Green DR (মার্চ ২০০০)। "The coordinate release of cytochrome c during apoptosis is rapid, complete and kinetically invariant"। Nature Cell Biology। 2 (3): 156–62। এসটুসিআইডি 2283955। ডিওআই:10.1038/35004029। পিএমআইডি 10707086।
- ↑ Lee JK, Lu S, Madhukar A (অক্টোবর ২০১০)। "Real-Time dynamics of Ca2+, caspase-3/7, and morphological changes in retinal ganglion cell apoptosis under elevated pressure"। PLOS ONE। 5 (10): e13437। ডিওআই:10.1371/journal.pone.0013437। পিএমআইডি 20976135। পিএমসি 2956638
 । বিবকোড:2010PLoSO...513437L।
। বিবকোড:2010PLoSO...513437L।
- ↑ Bejarano I, Espino J, González-Flores D, Casado JG, Redondo PC, Rosado JA, Barriga C, Pariente JA, Rodríguez AB (সেপ্টেম্বর ২০০৯)। "Role of Calcium Signals on Hydrogen Peroxide-Induced Apoptosis in Human Myeloid HL-60 Cells"। International Journal of Biomedical Science। 5 (3): 246–56। পিএমআইডি 23675144। পিএমসি 3614781
 ।
।
- ↑ Gonzalez, D.; Bejarano, I.; Barriga, C.; Rodriguez, A.B.; Pariente, J.A. (২০১০)। "Oxidative Stress-Induced Caspases are Regulated in Human Myeloid HL-60 Cells by Calcium Signal"। Current Signal Transduction Therapy। 5 (2): 181–186। ডিওআই:10.2174/157436210791112172।
- ↑ Mohan S, Abdul AB, Abdelwahab SI, Al-Zubairi AS, Sukari MA, Abdullah R, Elhassan Taha MM, Ibrahim MY, Syam S (অক্টোবর ২০১০)। "Typhonium flagelliforme induces apoptosis in CEMss cells via activation of caspase-9, PARP cleavage and cytochrome c release: its activation coupled with G0/G1 phase cell cycle arrest" (পিডিএফ)। Journal of Ethnopharmacology। 131 (3): 592–600। ডিওআই:10.1016/j.jep.2010.07.043। পিএমআইডি 20673794। ২০১৯-০৪-২৬ তারিখে মূল (পিডিএফ) থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০১৯-০৭-০৫।
- ↑ Brüne B (আগস্ট ২০০৩)। "Nitric oxide: NO apoptosis or turning it ON?"। Cell Death and Differentiation। 10 (8): 864–69। ডিওআই:10.1038/sj.cdd.4401261
 । পিএমআইডি 12867993।
। পিএমআইডি 12867993।
- ↑ Brüne B, von Knethen A, Sandau KB (অক্টোবর ১৯৯৯)। "Nitric oxide (NO): an effector of apoptosis"। Cell Death and Differentiation। 6 (10): 969–75। ডিওআই:10.1038/sj.cdd.4400582
 । পিএমআইডি 10556974।
। পিএমআইডি 10556974।
- ↑ Uren RT, Iyer S, Kluck RM (আগস্ট ২০১৭)। "Pore formation by dimeric Bak and Bax: an unusual pore?"। Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences। 372 (1726): 20160218। ডিওআই:10.1098/rstb.2016.0218। পিএমআইডি 28630157। পিএমসি 5483520
 ।
।
- ↑ Fesik SW, Shi Y (নভেম্বর ২০০১)। "Structural biology. Controlling the caspases"। Science। 294 (5546): 1477–78। এসটুসিআইডি 11392850। ডিওআই:10.1126/science.1062236। পিএমআইডি 11711663।
- ↑ ক খ Wajant H (মে ২০০২)। "The Fas signaling pathway: more than a paradigm"। Science। 296 (5573): 1635–36। এসটুসিআইডি 29449108। ডিওআই:10.1126/science.1071553। পিএমআইডি 12040174। বিবকোড:2002Sci...296.1635W।
- ↑ Chen G, Goeddel DV (মে ২০০২)। "TNF-R1 signaling: a beautiful pathway"। Science। 296 (5573): 1634–35। এসটুসিআইডি 25321662। ডিওআই:10.1126/science.1071924। পিএমআইডি 12040173। বিবকোড:2002Sci...296.1634C।
- ↑ Goeddel, DV (২০০৭)। "Connection Map for Tumor Necrosis Factor Pathway"। Science's STKE। 2007 (382): tw132। এসটুসিআইডি 85404086। ডিওআই:10.1126/stke.3822007tw132।
- ↑ Chen W, Li N, Chen T, Han Y, Li C, Wang Y, He W, Zhang L, Wan T, Cao X (ডিসেম্বর ২০০৫)। "The lysosome-associated apoptosis-inducing protein containing the pleckstrin homology (PH) and FYVE domains (LAPF), representative of a novel family of PH and FYVE domain-containing proteins, induces caspase-independent apoptosis via the lysosomal-mitochondrial pathway"। The Journal of Biological Chemistry। 280 (49): 40985–95। ডিওআই:10.1074/jbc.M502190200
 । পিএমআইডি 16188880।
। পিএমআইডি 16188880।
- ↑ Gerl R, Vaux DL (ফেব্রুয়ারি ২০০৫)। "Apoptosis in the development and treatment of cancer"। Carcinogenesis। 26 (2): 263–70। ডিওআই:10.1093/carcin/bgh283
 । পিএমআইডি 15375012।
। পিএমআইডি 15375012।
- ↑ Masum AA, Yokoi K, Hisamatsu Y, Naito K, Shashni B, Aoki S (সেপ্টেম্বর ২০১৮)। "Design and synthesis of a luminescent iridium complex-peptide hybrid (IPH) that detects cancer cells and induces their apoptosis"। Bioorganic & Medicinal Chemistry। 26 (17): 4804–16। ডিওআই:10.1016/j.bmc.2018.08.016। পিএমআইডি 30177492।
- ↑ Wajant H (২০০৭)। "Connection Map for Fas Signaling Pathway"। Science's STKE। 2007 (380): tr1। এসটুসিআইডি 84909531। ডিওআই:10.1126/stke.3802007tr1।
- ↑ Murphy KM, Ranganathan V, Farnsworth ML, Kavallaris M, Lock RB (জানুয়ারি ২০০০)। "Bcl-2 inhibits Bax translocation from cytosol to mitochondria during drug-induced apoptosis of human tumor cells"। Cell Death and Differentiation। 7 (1): 102–11। ডিওআই:10.1038/sj.cdd.4400597
 । পিএমআইডি 10713725।
। পিএমআইডি 10713725।
- ↑ Susin SA, Lorenzo HK, Zamzami N, Marzo I, Snow BE, Brothers GM, Mangion J, Jacotot E, Costantini P, Loeffler M, Larochette N, Goodlett DR, Aebersold R, Siderovski DP, Penninger JM, Kroemer G (ফেব্রুয়ারি ১৯৯৯)। "Molecular characterization of mitochondrial apoptosis-inducing factor"। Nature। 397 (6718): 441–46। এসটুসিআইডি 204991081। ডিওআই:10.1038/17135। পিএমআইডি 9989411। বিবকোড:1999Natur.397..441S।
- ↑ Jewhurst K, Levin M, McLaughlin KA (২০১৪)। "Optogenetic Control of Apoptosis in Targeted Tissues of Xenopus laevis Embryos"। Journal of Cell Death। 7: 25–31। ডিওআই:10.4137/JCD.S18368। পিএমআইডি 25374461। পিএমসি 4213186
 ।
।
- ↑ Venturi, Sebastiano (২০১১)। "Evolutionary Significance of Iodine"। Current Chemical Biology। 5 (3): 155–62। ডিওআই:10.2174/187231311796765012। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ Venturi, Sebastiano (২০১৪)। "Iodine, PUFAs and Iodolipids in Health and Disease: An Evolutionary Perspective"। Human Evolution। 29 (1–3): 185–205। আইএসএসএন 0393-9375।
- ↑ Tamura K, Takayama S, Ishii T, Mawaribuchi S, Takamatsu N, Ito M (জুন ২০১৫)। "Apoptosis and differentiation of Xenopus tail-derived myoblasts by thyroid hormone"। Journal of Molecular Endocrinology। 54 (3): 185–92। ডিওআই:10.1530/JME-14-0327
 । পিএমআইডি 25791374।
। পিএমআইডি 25791374।
- ↑ ক খ Jan R, Chaudhry G (২০১৯)। "Understanding Apoptosis and Apoptotic Pathways Targeted Cancer Therapeutics"। Advanced Pharmaceutical Bulletin। 9 (2): 205–218। ডিওআই:10.15171/apb.2019.024। পিএমআইডি 31380246। পিএমসি 6664112
 ।
।
- ↑ Kale J, Osterlund EJ, Andrews DW (২০১৮)। "BCL-2 family proteins: changing partners in the dance towards death"। Cell Death & Differentiation। 25 (1): 65–80। ডিওআই:10.1038/cdd.2017.186। পিএমআইডি 29149100। পিএমসি 5729540
 ।
।
- ↑ Razaghi A, Heimann K, Schaeffer PM, Gibson SB (ফেব্রুয়ারি ২০১৮)। "Negative regulators of cell death pathways in cancer: perspective on biomarkers and targeted therapies"। Apoptosis। 23 (2): 93–112। এসটুসিআইডি 3424489। ডিওআই:10.1007/s10495-018-1440-4। পিএমআইডি 29322476।
- ↑ Thomas MP, Liu X, Whangbo J, McCrossan G, Sanborn KB, Basar E, Walch M, Lieberman J (মে ২০১৫)। "Apoptosis Triggers Specific, Rapid, and Global mRNA Decay with 3' Uridylated Intermediates Degraded by DIS3L2"। Cell Reports। 11 (7): 1079–89। ডিওআই:10.1016/j.celrep.2015.04.026। পিএমআইডি 25959823। পিএমসি 4862650
 ।
।
- ↑ Böhm I (২০০৩)। "Disruption of the cytoskeleton after apoptosis induction by autoantibodies"। Autoimmunity। 36 (3): 183–89। এসটুসিআইডি 37887253। ডিওআই:10.1080/0891693031000105617। পিএমআইডি 12911286।
- ↑ Susin SA, Daugas E, Ravagnan L, Samejima K, Zamzami N, Loeffler M, ও অন্যান্য (আগস্ট ২০০০)। "Two distinct pathways leading to nuclear apoptosis"। The Journal of Experimental Medicine। 192 (4): 571–80। ডিওআই:10.1084/jem.192.4.571। পিএমআইডি 10952727। পিএমসি 2193229
 ।
।
- ↑ Kihlmark M, Imreh G, Hallberg E (অক্টোবর ২০০১)। "Sequential degradation of proteins from the nuclear envelope during apoptosis"। Journal of Cell Science। 114 (Pt 20): 3643–53। পিএমআইডি 11707516।
- ↑ Nagata S (এপ্রিল ২০০০)। "Apoptotic DNA fragmentation"। Experimental Cell Research। 256 (1): 12–8। ডিওআই:10.1006/excr.2000.4834। পিএমআইডি 10739646।
- ↑ Gong J, Traganos F, Darzynkiewicz Z (মে ১৯৯৪)। "A selective procedure for DNA extraction from apoptotic cells applicable for gel electrophoresis and flow cytometry"। Analytical Biochemistry। 218 (2): 314–19। ডিওআই:10.1006/abio.1994.1184। পিএমআইডি 8074286।
- ↑ Iwata M, Myerson D, Torok-Storb B, Zager RA (ডিসেম্বর ১৯৯৪)। "An evaluation of renal tubular DNA laddering in response to oxygen deprivation and oxidant injury"। Journal of the American Society of Nephrology। 5 (6): 1307–13। পিএমআইডি 7893995।
- ↑ Smith, Aaron; Parkes, Michael AF; Atkin-Smith, Georgia K; Tixeira, Rochelle; Poon, Ivan KH (২০১৭)। "Cell disassembly during apoptosis"। WikiJournal of Medicine (ইংরেজি ভাষায়)। 4 (1)। ডিওআই:10.15347/wjm/2017.008
 । অজানা প্যারামিটার
। অজানা প্যারামিটার |name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ ক খ Tixeira R, Caruso S, Paone S, Baxter AA, Atkin-Smith GK, Hulett MD, Poon IK (মার্চ ২০১৭)। "Defining the morphologic features and products of cell disassembly during apoptosis"। Apoptosis। 22 (3): 475–77। এসটুসিআইডি 34648758। ডিওআই:10.1007/s10495-017-1345-7। পিএমআইডি 28102458।
- ↑ Coleman ML, Sahai EA, Yeo M, Bosch M, Dewar A, Olson MF (এপ্রিল ২০০১)। "Membrane blebbing during apoptosis results from caspase-mediated activation of ROCK I"। Nature Cell Biology। 3 (4): 339–45। এসটুসিআইডি 2537726। ডিওআই:10.1038/35070009। পিএমআইডি 11283606।
- ↑ Sebbagh M, Renvoizé C, Hamelin J, Riché N, Bertoglio J, Bréard J (এপ্রিল ২০০১)। "Caspase-3-mediated cleavage of ROCK I induces MLC phosphorylation and apoptotic membrane blebbing"। Nature Cell Biology। 3 (4): 346–52। এসটুসিআইডি 36187702। ডিওআই:10.1038/35070019। পিএমআইডি 11283607।
- ↑ Moss DK, Betin VM, Malesinski SD, Lane JD (জুন ২০০৬)। "A novel role for microtubules in apoptotic chromatin dynamics and cellular fragmentation"। Journal of Cell Science। 119 (Pt 11): 2362–74। ডিওআই:10.1242/jcs.02959। পিএমআইডি 16723742। পিএমসি 1592606
 ।
।
- ↑ ক খ Poon IK, Chiu YH, Armstrong AJ, Kinchen JM, Juncadella IJ, Bayliss DA, Ravichandran KS (মার্চ ২০১৪)। "Unexpected link between an antibiotic, pannexin channels and apoptosis"। Nature। 507 (7492): 329–34। ডিওআই:10.1038/nature13147। পিএমআইডি 24646995। পিএমসি 4078991
 । বিবকোড:2014Natur.507..329P।
। বিবকোড:2014Natur.507..329P।
- ↑ Atkin-Smith GK, Tixeira R, Paone S, Mathivanan S, Collins C, Liem M, Goodall KJ, Ravichandran KS, Hulett MD, Poon IK (জুন ২০১৫)। "A novel mechanism of generating extracellular vesicles during apoptosis via a beads-on-a-string membrane structure"। Nature Communications। 6: 7439। ডিওআই:10.1038/ncomms8439। পিএমআইডি 26074490। পিএমসি 4490561
 । বিবকোড:2015NatCo...6.7439A।
। বিবকোড:2015NatCo...6.7439A।
- ↑ Vandivier RW, Henson PM, Douglas IS (জুন ২০০৬)। "Burying the dead: the impact of failed apoptotic cell removal (efferocytosis) on chronic inflammatory lung disease"। Chest। 129 (6): 1673–82। ডিওআই:10.1378/chest.129.6.1673। পিএমআইডি 16778289।
- ↑ Li MO, Sarkisian MR, Mehal WZ, Rakic P, Flavell RA (নভেম্বর ২০০৩)। "Phosphatidylserine receptor is required for clearance of apoptotic cells"। Science। 302 (5650): 1560–63। এসটুসিআইডি 36252352। ডিওআই:10.1126/science.1087621। পিএমআইডি 14645847। বিবকোড:2003Sci...302.1560O।
- ↑ Wang X, Wu YC, Fadok VA, Lee MC, Gengyo-Ando K, Cheng LC, ও অন্যান্য (নভেম্বর ২০০৩)। "Cell corpse engulfment mediated by C. elegans phosphatidylserine receptor through CED-5 and CED-12"। Science। 302 (5650): 1563–66। এসটুসিআইডি 25672278। ডিওআই:10.1126/science.1087641। পিএমআইডি 14645848। বিবকোড:2003Sci...302.1563W।
- ↑ Savill J, Gregory C, Haslett C (নভেম্বর ২০০৩)। "Cell biology. Eat me or die"। Science। 302 (5650): 1516–17। hdl:1842/448
 । এসটুসিআইডি 13402617। ডিওআই:10.1126/science.1092533। পিএমআইডি 14645835।
। এসটুসিআইডি 13402617। ডিওআই:10.1126/science.1092533। পিএমআইডি 14645835।
- ↑ Krysko DV, Vandenabeele P (২০০৯-০১-১৪)। Phagocytosis of dying cells: from molecular mechanisms to human diseases। Springer। আইএসবিএন 978-1-4020-9292-3।
- ↑ Halicka HD, Bedner E, Darzynkiewicz Z (নভেম্বর ২০০০)। "Segregation of RNA and separate packaging of DNA and RNA in apoptotic bodies during apoptosis"। Experimental Cell Research। 260 (2): 248–56। ডিওআই:10.1006/excr.2000.5027। পিএমআইডি 11035919।
- ↑ Lozano GM, Bejarano I, Espino J, González D, Ortiz A, García JF, Rodríguez AB, Pariente JA (২০০৯)। "Density gradient capacitation is the most suitable method to improve fertilization and to reduce DNA fragmentation positive spermatozoa of infertile men"। Anatolian Journal of Obstetrics & Gynecology। 3 (1): 1–7।
- ↑ Darzynkiewicz Z, Juan G, Li X, Gorczyca W, Murakami T, Traganos F (জানুয়ারি ১৯৯৭)। "Cytometry in cell necrobiology: analysis of apoptosis and accidental cell death (necrosis)"। Cytometry। 27 (1): 1–20। ডিওআই:10.1002/(sici)1097-0320(19970101)27:1<1::aid-cyto2>3.0.co;2-l
 । পিএমআইডি 9000580।
। পিএমআইডি 9000580।
- ↑ Krysko DV, Vanden Berghe T, Parthoens E, D'Herde K, Vandenabeele P (২০০৮)। Methods for distinguishing apoptotic from necrotic cells and measuring their clearance। Methods in Enzymology। 442। পৃষ্ঠা 307–41। আইএসবিএন 9780123743121। ডিওআই:10.1016/S0076-6879(08)01416-X। পিএমআইডি 18662577।
- ↑ Krysko DV, Vanden Berghe T, D'Herde K, Vandenabeele P (মার্চ ২০০৮)। "Apoptosis and necrosis: detection, discrimination and phagocytosis"। Methods। 44 (3): 205–21। ডিওআই:10.1016/j.ymeth.2007.12.001। পিএমআইডি 18314051।
- ↑ Vanden Berghe T, Grootjans S, Goossens V, Dondelinger Y, Krysko DV, Takahashi N, Vandenabeele P (জুন ২০১৩)। "Determination of apoptotic and necrotic cell death in vitro and in vivo"। Methods। 61 (2): 117–29। ডিওআই:10.1016/j.ymeth.2013.02.011। পিএমআইডি 23473780। ২০১৯-১১-০৫ তারিখে মূল থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০১৯-১১-০৫।
- ↑ Wlodkowic D, Telford W, Skommer J, Darzynkiewicz Z (২০১১)। "Apoptosis and beyond: cytometry in studies of programmed cell death"। Recent Advances in Cytometry, Part B - Advances in Applications। Methods in Cell Biology। 103। পৃষ্ঠা 55–98। আইএসবিএন 9780123854933। ডিওআই:10.1016/B978-0-12-385493-3.00004-8। পিএমআইডি 21722800। পিএমসি 3263828
 ।
।
- ↑ Thompson CB (মার্চ ১৯৯৫)। "Apoptosis in the pathogenesis and treatment of disease"। Science। 267 (5203): 1456–62। এসটুসিআইডি 12991980। ডিওআই:10.1126/science.7878464। পিএমআইডি 7878464। বিবকোড:1995Sci...267.1456T।
- ↑ Yang L, Mashima T, Sato S, Mochizuki M, Sakamoto H, Yamori T, Oh-Hara T, Tsuruo T (ফেব্রুয়ারি ২০০৩)। "Predominant suppression of apoptosome by inhibitor of apoptosis protein in non-small cell lung cancer H460 cells: therapeutic effect of a novel polyarginine-conjugated Smac peptide"। Cancer Research। 63 (4): 831–37। পিএমআইডি 12591734।
- ↑ Vlahopoulos SA (আগস্ট ২০১৭)। "Aberrant control of NF-κB in cancer permits transcriptional and phenotypic plasticity, to curtail dependence on host tissue: molecular mode"। Cancer Biology & Medicine। 14 (3): 254–70। ডিওআই:10.20892/j.issn.2095-3941.2017.0029। পিএমআইডি 28884042। পিএমসি 5570602
 ।
।
- ↑ Takaoka A, Hayakawa S, Yanai H, Stoiber D, Negishi H, Kikuchi H, ও অন্যান্য (জুলাই ২০০৩)। "Integration of interferon-alpha/beta signalling to p53 responses in tumour suppression and antiviral defence"। Nature। 424 (6948): 516–23। ডিওআই:10.1038/nature01850
 । পিএমআইডি 12872134। বিবকোড:2003Natur.424..516T।
। পিএমআইডি 12872134। বিবকোড:2003Natur.424..516T।
- ↑ Bernstein C, Bernstein H, Payne CM, Garewal H (জুন ২০০২)। "DNA repair/pro-apoptotic dual-role proteins in five major DNA repair pathways: fail-safe protection against carcinogenesis"। Mutation Research। 511 (2): 145–78। ডিওআই:10.1016/S1383-5742(02)00009-1। পিএমআইডি 12052432।
- ↑ ক খ Kaczanowski S (২০১৬)। "Apoptosis: its origin, history, maintenance and the medical implications for cancer and aging" (পিডিএফ)। Phys Biol। 13 (3): 031001। ডিওআই:10.1088/1478-3975/13/3/031001। পিএমআইডি 27172135। বিবকোড:2016PhBio..13c1001K। ২০১৯-০৪-২৮ তারিখে মূল (পিডিএফ) থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০১৯-১২-২৬।
- ↑ Warburg O (ফেব্রুয়ারি ১৯৫৬)। "On the origin of cancer cells"। Science। 123 (3191): 309–14। ডিওআই:10.1126/science.123.3191.309। পিএমআইডি 13298683। বিবকোড:1956Sci...123..309W।
- ↑ ক খ গ ঘ ঙ চ Del Puerto HL, Martins AS, Milsted A, Souza-Fagundes EM, Braz GF, Hissa B, Andrade LO, Alves F, Rajão DS, Leite RC, Vasconcelos AC (জুন ২০১১)। "Canine distemper virus induces apoptosis in cervical tumor derived cell lines"। Virology Journal। 8 (1): 334। ডিওআই:10.1186/1743-422X-8-334। পিএমআইডি 21718481। পিএমসি 3141686
 ।
।
- ↑ Liu HC, Chen GG, Vlantis AC, Tse GM, Chan AT, van Hasselt CA (মার্চ ২০০৮)। "Inhibition of apoptosis in human laryngeal cancer cells by E6 and E7 oncoproteins of human papillomavirus 16"। Journal of Cellular Biochemistry। 103 (4): 1125–43। এসটুসিআইডি 1651475। ডিওআই:10.1002/jcb.21490। পিএমআইডি 17668439।
- ↑ ক খ Niu XY, Peng ZL, Duan WQ, Wang H, Wang P (২০০৬)। "Inhibition of HPV 16 E6 oncogene expression by RNA interference in vitro and in vivo"। International Journal of Gynecological Cancer। 16 (2): 743–51। ডিওআই:10.1111/j.1525-1438.2006.00384.x। পিএমআইডি 16681755।
- ↑ ক খ Liu Y, McKalip A, Herman B (মে ২০০০)। "Human papillomavirus type 16 E6 and HPV-16 E6/E7 sensitize human keratinocytes to apoptosis induced by chemotherapeutic agents: roles of p53 and caspase activation"। Journal of Cellular Biochemistry। 78 (2): 334–49। ডিওআই:10.1002/(sici)1097-4644(20000801)78:2<334::aid-jcb15>3.3.co;2-6। পিএমআইডি 10842327।
- ↑ Boehm I (জুন ২০০৬)। "Apoptosis in physiological and pathological skin: implications for therapy"। Current Molecular Medicine। 6 (4): 375–94। ডিওআই:10.2174/156652406777435390। পিএমআইডি 16900661।
- ↑ LaFerla FM, Tinkle BT, Bieberich CJ, Haudenschild CC, Jay G (জানুয়ারি ১৯৯৫)। "The Alzheimer's A beta peptide induces neurodegeneration and apoptotic cell death in transgenic mice"। Nature Genetics। 9 (1): 21–30। এসটুসিআইডি 20016461। ডিওআই:10.1038/ng0195-21। পিএমআইডি 7704018।
- ↑ Mochizuki H, Goto K, Mori H, Mizuno Y (মে ১৯৯৬)। "Histochemical detection of apoptosis in Parkinson's disease"। Journal of the Neurological Sciences। 137 (2): 120–3। এসটুসিআইডি 44329454। ডিওআই:10.1016/0022-510X(95)00336-Z। পিএমআইডি 8782165।
- ↑ Demetrius LA, Magistretti PJ, Pellerin L (২০১৪)। "Alzheimer's disease: the amyloid hypothesis and the Inverse Warburg effect"। Frontiers in Physiology। 5: 522। ডিওআই:10.3389/fphys.2014.00522। পিএমআইডি 25642192। পিএমসি 4294122
 ।
।
- ↑ Musicco M, Adorni F, Di Santo S, Prinelli F, Pettenati C, Caltagirone C, Palmer K, Russo A (জুলাই ২০১৩)। "Inverse occurrence of cancer and Alzheimer disease: a population-based incidence study"। Neurology। 81 (4): 322–8। এসটুসিআইডি 22792702। ডিওআই:10.1212/WNL.0b013e31829c5ec1। পিএমআইডি 23843468।
- ↑ Farhana L, Dawson MI, Fontana JA (জুন ২০০৫)। "Apoptosis induction by a novel retinoid-related molecule requires nuclear factor-kappaB activation"। Cancer Research। 65 (11): 4909–17। ডিওআই:10.1158/0008-5472.CAN-04-4124
 । পিএমআইডি 15930313।
। পিএমআইডি 15930313।
- ↑ Alimonti JB, Ball TB, Fowke KR (জুলাই ২০০৩)। "Mechanisms of CD4+ T lymphocyte cell death in human immunodeficiency virus infection and AIDS"। The Journal of General Virology। 84 (Pt 7): 1649–61। ডিওআই:10.1099/vir.0.19110-0
 । পিএমআইডি 12810858।
। পিএমআইডি 12810858।
- ↑ Vashistha, Himanshu; Husain, Mohammad; Kumar, Dileep; Yadav, Anju; Arora, Shitij; Singhal, Pravin C. (২০০৮)। "HIV-1 Expression Induces Tubular Cell G2/M Arrest and Apoptosis"। Renal Failure। 30 (6): 655–664। ডিওআই:10.1080/08860220802134672
 । পিএমআইডি 18661417।
। পিএমআইডি 18661417।
- ↑ Indiana University Health। "AIDS Defining Criteria | Riley"। IU Health। ২০১৩-০৫-২৬ তারিখে মূল থেকে আর্কাইভ করা। সংগ্রহের তারিখ ২০১৩-০১-২০।
- ↑ Tateishi H, Monde K, Anraku K, Koga R, Hayashi Y, Ciftci HI, DeMirci H, Higashi T, Motoyama K, Arima H, Otsuka M, Fujita M (আগস্ট ২০১৭)। "A clue to unprecedented strategy to HIV eradication: "Lock-in and apoptosis""। Scientific Reports। 7 (1): 8957। ডিওআই:10.1038/s41598-017-09129-w। পিএমআইডি 28827668। পিএমসি 5567282
 । বিবকোড:2017NatSR...7.8957T।
। বিবকোড:2017NatSR...7.8957T।
- ↑ ক খ Indran IR, Tufo G, Pervaiz S, Brenner C (জুন ২০১১)। "Recent advances in apoptosis, mitochondria and drug resistance in cancer cells"। Biochimica et Biophysica Acta (BBA) - Bioenergetics। 1807 (6): 735–45। ডিওআই:10.1016/j.bbabio.2011.03.010। পিএমআইডি 21453675।
- ↑ Everett H, McFadden G (এপ্রিল ১৯৯৯)। "Apoptosis: an innate immune response to virus infection"। Trends in Microbiology। 7 (4): 160–65। ডিওআই:10.1016/S0966-842X(99)01487-0। পিএমআইডি 10217831।
- ↑ Nishi T, Tsukiyama-Kohara K, Togashi K, Kohriyama N, Kai C (নভেম্বর ২০০৪)। "Involvement of apoptosis in syncytial cell death induced by canine distemper virus"। Comparative Immunology, Microbiology and Infectious Diseases। 27 (6): 445–55। ডিওআই:10.1016/j.cimid.2004.01.007। পিএমআইডি 15325517।
- ↑ ক খ গ ঘ Acrani GO, Gomes R, Proença-Módena JL, da Silva AF, Carminati PO, Silva ML, Santos RI, Arruda E (এপ্রিল ২০১০)। "Apoptosis induced by Oropouche virus infection in HeLa cells is dependent on virus protein expression"। Virus Research। 149 (1): 56–63। ডিওআই:10.1016/j.virusres.2009.12.013। পিএমআইডি 20080135।
- ↑ Azevedo RS, Nunes MR, Chiang JO, Bensabath G, Vasconcelos HB, Pinto AY, Martins LC, Monteiro HA, Rodrigues SG, Vasconcelos PF (জুন ২০০৭)। "Reemergence of Oropouche fever, northern Brazil"। Emerging Infectious Diseases। 13 (6): 912–15। ডিওআই:10.3201/eid1306.061114। পিএমআইডি 17553235। পিএমসি 2792853
 ।
।
- ↑ Santos RI, Rodrigues AH, Silva ML, Mortara RA, Rossi MA, Jamur MC, Oliver C, Arruda E (ডিসেম্বর ২০০৮)। "Oropouche virus entry into HeLa cells involves clathrin and requires endosomal acidification"। Virus Research। 138 (1–2): 139–43। ডিওআই:10.1016/j.virusres.2008.08.016। পিএমআইডি 18840482। পিএমসি 7114418

|pmc=এর মান পরীক্ষা করুন (সাহায্য)। - ↑ Teodoro JG, Branton PE (মার্চ ১৯৯৭)। "Regulation of apoptosis by viral gene products"। Journal of Virology। 71 (3): 1739–46। ডিওআই:10.1128/jvi.71.3.1739-1746.1997। পিএমআইডি 9032302। পিএমসি 191242
 ।
।
- ↑ Polster BM, Pevsner J, Hardwick JM (মার্চ ২০০৪)। "Viral Bcl-2 homologs and their role in virus replication and associated diseases"। Biochimica et Biophysica Acta (BBA) - Molecular Cell Research। 1644 (2–3): 211–27। ডিওআই:10.1016/j.bbamcr.2003.11.001। পিএমআইডি 14996505।
- ↑ ক খ Hay S, Kannourakis G (জুলাই ২০০২)। "A time to kill: viral manipulation of the cell death program"। The Journal of General Virology। 83 (Pt 7): 1547–64। ডিওআই:10.1099/0022-1317-83-7-1547। পিএমআইডি 12075073। সাইট সিয়ারX 10.1.1.322.6923
 ।
।
- ↑ Wang XW, Gibson MK, Vermeulen W, Yeh H, Forrester K, Stürzbecher HW, Hoeijmakers JH, Harris CC (ডিসেম্বর ১৯৯৫)। "Abrogation of p53-induced apoptosis by the hepatitis B virus X gene"। Cancer Research। 55 (24): 6012–16। পিএমআইডি 8521383।
- ↑ Collazo, Cyrelys; Chacón, Osmani; Borrás, Orlando (২০০৬)। "Programmed cell death in plants resembles apoptosis of animals" (পিডিএফ)। Biotecnología Aplicada। 23: 1–10। ২০০৯-০৩-০৩ তারিখে মূল (পিডিএফ) থেকে আর্কাইভ করা। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য) - ↑ Dickman, Martin; Williams, Brett; Li, Yurong; De Figueiredo, Paul; Wolpert, Thomas (২০১৭)। "Reassessing apoptosis in plants"। Nature Plants। 3 (10): 773–779। এসটুসিআইডি 3290201। ডিওআই:10.1038/s41477-017-0020-x। পিএমআইডি 28947814।
- ↑ Xiang J, Chao DT, Korsmeyer SJ (ডিসেম্বর ১৯৯৬)। "BAX-induced cell death may not require interleukin 1 beta-converting enzyme-like proteases"। Proceedings of the National Academy of Sciences of the United States of America। 93 (25): 14559–63। ডিওআই:10.1073/pnas.93.25.14559। পিএমআইডি 8962091। পিএমসি 26172
 । বিবকোড:1996PNAS...9314559X।
। বিবকোড:1996PNAS...9314559X।
- ↑ Kim, Jin Hee; Lee, C. H. (২০০৯)। "Atromentin-Induced Apoptosis in Human Leukemia U937 Cells"। Journal of Microbiology and Biotechnology। 19 (9): 946–950। এসটুসিআইডি 11552839। ডিওআই:10.4014/jmb.0811.617। পিএমআইডি 19809251।
General bibliography
- Alberts, Bruce; Johnson, Alexander; Lewis, Julian; Morgan, David; Raff, Martin; Roberts, Keith; Walter, Peter (২০১৫)। Molecular Biology of the Cell (6th সংস্করণ)। Garland Science। পৃষ্ঠা 2। আইএসবিএন 978-0815344322। অজানা প্যারামিটার
|name-list-style=উপেক্ষা করা হয়েছে (সাহায্য)
External links
- Apoptosis & cell surface[স্থায়ীভাবে অকার্যকর সংযোগ]
- Apoptosis & Caspase 3, The Proteolysis Map – animation
- Apoptosis & Caspase 8, The Proteolysis Map – animation
- Apoptosis & Caspase 7, The Proteolysis Map – animation
- Apoptosis MiniCOPE Dictionary – list of apoptosis terms and acronyms
- Apoptosis (Programmed Cell Death) – The Virtual Library of Biochemistry, Molecular Biology and Cell Biology
- Apoptosis Research Portal
- Apoptosis Info Apoptosis protocols, articles, news, and recent publications.
- Database of proteins involved in apoptosis
- Apoptosis Video
- Apoptosis Video (WEHI on YouTube )
- The Mechanisms of Apoptosis Kimball's Biology Pages. Simple explanation of the mechanisms of apoptosis triggered by internal signals (bcl-2), along the caspase-9, caspase-3 and caspase-7 pathway; and by external signals (FAS and TNF), along the caspase 8 pathway. Accessed 25 March 2007.
- WikiPathways – Apoptosis pathway
- "Finding Cancer's Self-Destruct Button". CR magazine (Spring 2007). Article on apoptosis and cancer.
- Xiaodong Wang's lecture: Introduction to Apoptosis
- Robert Horvitz's Short Clip: Discovering Programmed Cell Death
- The Bcl-2 Database
- DeathBase: a database of proteins involved in cell death, curated by experts
- European Cell Death Organization
- Apoptosis signaling pathway created by Cusabio
টেমপ্লেট:Cell cycle proteins টেমপ্লেট:Signal transduction টেমপ্লেট:Apoptosis signaling pathway


